
Testimonials
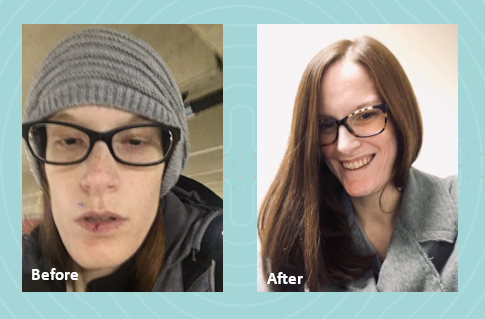
In 2022, I graduated from nursing school with dreams of starting my career as a nurse. However, life had other plans. I was diagnosed with gastroparesis, a condition that made it impossible for me to work and pursue my passion. As my condition worsened, I had to put my career on hold to focus on my health.
 Initially, my local clinicians recommended jejunal feedings, which I tolerated well at first. However, after my J-tube surgery, my condition began to deteriorate, and eventually I became severely malnourished. I was surviving on a mere 500 calories a day, leaving me too weak to perform even the simplest tasks. My mom had to help me with everything, including bathing. Living in a two-story home became a daily struggle, as I had to crawl up the stairs, feeling my body slowly giving up.
Initially, my local clinicians recommended jejunal feedings, which I tolerated well at first. However, after my J-tube surgery, my condition began to deteriorate, and eventually I became severely malnourished. I was surviving on a mere 500 calories a day, leaving me too weak to perform even the simplest tasks. My mom had to help me with everything, including bathing. Living in a two-story home became a daily struggle, as I had to crawl up the stairs, feeling my body slowly giving up.
My local registered dietitian recommended Parenteral Nutrition (PN) and sent the order. We were then referred to Option Care Health (OPCH). I was scared to start PN, but my OPCH dietitian reassured me, saying, “Just because you’re on PN doesn’t mean your life is over. The goal is to give you back more of your life than before.” Her words stuck with me, offering hope during a difficult time.
Due to my blood sugar issues, I’m on 23-hour PN feeds and carry a backpack that has become a part of me. Despite these challenges, my OPCH team has been incredible. My registered dietitian and pharmacist have truly been lifesavers. I continue to speak with my OPCH registered dietitian weekly because she genuinely cares about my well-being and supports me through every step of my journey.
Thanks to the unwavering support of my Option Care Health team and my local registered dietitian, I am back to work and feeling so much better. I wholeheartedly recommend Option Care Health to anyone in need. They have played a crucial role in my recovery, and I am forever grateful for their dedication and care.

Testimonials
Gillian was just 11 years old when she began treatment for multiple complex chronic illnesses. As a teenager, she was diagnosed with gastrointestinal (GI) motility disorder and gastroparesis, which led to long-term, severe malnutrition.
“It was really hard missing out on so many activities growing up. I was prescribed various medications and tube feedings, but nothing helped long term. By early adulthood my symptoms worsened so I had to withdraw from college and take an extended medical leave from my job,” she said.
From 2015 to 2018, Gillian’s health progressively declined. “I was on tube feeds and other intravenous (IV) medications at the time. I began losing weight again, my neurological function was declining and I couldn’t speak or walk.” As Gillian’s health continued to decline, she found the strength to advocate for herself and build upon her excellent team of healthcare providers.
Gillian was put on total parenteral nutrition (TPN) in 2018, managed by Option Care Health. “This was my turning point. Today my labs are perfect and my cognitive function is back to normal. My weight has stabilized and I’m back to living life. I owe so much of my progress to my Option Care Health team.” Gillian continued, “My registered dietitian (RD) is amazing. During the initial COVID outbreak, I was struggling with my health and I couldn’t reach my doctors, but my Option Care Health RD was there every time I reached out. I got the help I needed and I owe it all to her.”
She claims that her Option Care Health team including her pharmacist and pharmacy technician go above and beyond expectation. “Other companies and even providers don’t always focus on how the patient needs to be living their best quality of life during treatment. My team at Option Care Health set up my deliveries in the evening to accommodate my work schedule. They also deliver them upstairs to me because I’m unable to carry them. My pharmacist and tech were so helpful this summer. They were able to find a way for me to go on vacation by switching around my infusions and supplies. Thanks to their help, I was able to go on my first trip since 2015! They are really focused on me as a person, not just a patient.”
Her message to her Option Care Health team is one of gratitude, “I just want them all to know how appreciative I am. They have and continue to be a key part of my recovery and I couldn’t be more grateful.” Gillian is thriving and living her best quality of life. She’s working, volunteering and spending as much time as possible with family and friends.
Learn more about malnutrition and join us in spreading awareness this ASPEN Malnutrition Awareness Week*, September 19th-23rd: ASPENMAW22
*Malnutrition Awareness Week™ is a mark of the American Society for Parenteral and Enteral Nutrition (ASPEN). Used with permission from ASPEN.

Testimonials
Four years ago, Sherry Hambly, 56, developed a painful rash, that constantly felt as if she had a terrible sunburn. Her skin burned every time she washed her hands or took a shower and her muscles were weak. After a long journey searching for answers, she was diagnosed with dermatomyositis, an autoimmune disorder. She’s now receiving intravenous immunoglobulin (IVIG) at the Option Care Health Infusion Suite in Troy, Mich., and is grateful to have her life back.
Prior to finding the right diagnosis and treatment, Sherry was so uncomfortable she had to take pain medicine daily and could barely perform her job as an accountant, due to weakness. She didn’t sleep well and was too exhausted to relish the things that brought her joy, including playing with her grandchildren, golfing, bowling and doing yoga.
“I love the employees at the Troy infusion suite because I never have to lift a finger – they take care of everything and made sure my care plan was personalized for me,” said Sherry, of Rochester Hills, Mich.
Early on, she was taking hydroxychloroquine, a high dose of steroids and an anti-rejection drug. Her original IVIG prescription involved four-hour IVIG infusions three days in a row once a month, but by the end of the month the benefits wore off and she didn’t have the energy to go to the office. The Option Care Health team worked with Sherry, her doctor and pharmacist to devise a care plan that worked best for her and she now receives the infusions two days a week every other week.
“It’s made all the difference in the world,” she said. “I no longer take any pain pills and am completely off all the steroids I relied on to keep me moving, because my IVIG treatment is helping so dramatically.”
She lives with her husband, son and two grandchildren. Now that she has her energy back, she’s able to assist her 11-year-old grandson with his home schooling and watch her 16-month old granddaughter. She’s back to golfing and doing yoga and can perform her job to her fullest potential.
“I really like the infusion suite – it’s nice being in your own little space during COVID-19 – the room has windows, comfortable chairs and a kitchen where I can warm up my coffee. It’s quiet and I can even work while I’m there,” she said. “The staff is always going above and beyond to make sure we’re safe and comfortable.”

Testimonials
Frequently ill with pneumonia, bronchitis and other serious infections, Cambria Hooven, 35, limited her contact with people and didn’t leave her house much. After finally learning the reason for her near-constant sickness was a weakened immune system due to common variable immune deficiency (CVID), she began receiving intravenous immunoglobulin (IVIG) at home through Option Care Health. She felt free to get out more and socialize, but then the COVID-19 pandemic hit.
Because Cambria was afraid to risk having visitors come to her home, her Option Care Health nurse, Kola devised a plan. He suggested she receive treatments at the Option Care Health Langhorne Infusion Suite where he works, which is a 35-minute drive from her home in Philadelphia.
“I was nervous about it as I hesitate to go anywhere during this pandemic, so he sent me a video of the suite before my first appointment, walking through everything and showing me exactly what doors to enter,” said Cambria, who gets teary eyed at the memory. “Kola has been my nurse for two years and he’s like family to me. I don’t know what I would do without him in my life!”
She now receives her four-hour monthly treatments in a clean and sanitized room, which has its own comfortable lounge chair and large windows. Because she otherwise stays home during the pandemic, she really enjoys going for her monthly infusions. “It’s a little retreat center,” says Cambria.
Cambria is relieved to finally have a diagnosis and receive treatment. For years, she saw one doctor after the next to try to figure out why she was always sick. Eight years ago, she had her appendix removed, got a serious blood infection and spent 33 days in the hospital, unsure if she would survive. Determined to get to the bottom of her problem, she took a leave from her job as a social worker in child welfare to have one test after the other.
She finally saw an immune specialist who diagnosed her condition and prescribed IVIG. As a result, she hasn’t been hospitalized since. Initially, she began self-infusing at home, but wasn’t comfortable with it. Option Care Health recommended a nurse come to her home to provide the infusions and that’s how she met Kola.
Now that she’s receiving treatment, Cambria feels healthier and is able to do her work as a social worker remotely, often from the Langhorne infusion suite.
“I know how to stay safe and the treatment I get at Option Care Health helps so I don’t have to live in fear and isolation. I can get outside safely to hike and backpack,” she said. “It’s great going to the Langhorne suite, which is safe and clean and I have so much respect for the nurses and their families. They’re so considerate.”

Testimonials
Abbi Tucker’s simple wish is to be a normal teenager and enjoy playing music, but when she was 13, severe migraine headaches and terrible stomach aches, that resulted in a 50-pound weight loss, derailed her hopes for a while. After numerous tests and consultations with doctors she was diagnosed with Crohn’s disease, an inflammatory bowel disease. Her life is back on track now that she receives infusions of therapy treating chronic inflammatory disorders at Option Care Health’s Troy Infusion Suite.
“Once I started getting treatment, my life changed,” says Abbi, now 16, of Marysville, Mich. “I gained the weight back and could finally focus on school and having fun again.”
When Abbi started experiencing severe health issues, she and her family were frightened and she was miserable. Her symptoms caused her to miss at least one day of school a week and she found it difficult to keep up with her studies. She couldn’t hang out with her friends, play or teach piano, and even lost her appetite.
Now with a treatment plan in place, she’s back to her activities, including band practice as a junior drum major, spending time with friends and playing music at her church. Eating is also gratifying, although she stays away from greasy and spicy foods as well as popcorn.
Abbi originally received her one-hour therapy every seven weeks at the hospital. When insurance issues arose necessitating a switch to an infusion company, she and her family selected Option Care Health and couldn’t be happier with their choice.
“I LOVE the nurses there,” she said. “I have a hard time getting my blood going for blood draws, which made them painful. One of my Option Care Health infusion nurses made me a heating pad and I use it every time I get my blood drawn. It’s amazing.”
Antonette, the receptionist at the facility, calls to remind her family about upcoming appointments and the staff knows to look for her dad’s red truck when she gets dropped off. He’s a fireman and paramedic with a medical background, which puts her family at ease.
She likes getting her care at the infusion suite instead of at home because she occasionally has had adverse reactions. She takes Benadryl and a steroid before every treatment, which helps, but she’s comforted to know that Option Care Health nurses are nearby if she starts having issues. She also appreciates the privacy of the suites.
“The staff always makes me feel right at home and that my health is their number one priority,” said Abbi. “Infusion therapy really has been lifechanging and now I can do what a typical 16-year-old would do every day.”

Testimonials
October 18-24 is National Pharmacy Week. Each year we celebrate Pharmacy Week to acknowledge the invaluable contributions that pharmacists and technicians make to improve patient care throughout the care spectrum. We recently sat down with a few members of our pharmacy team to learn more about their experience in pharmacy and working at Option Care Health. Keep reading to learn more about:
- Jamie Broome, Pharmacy Technician Supervisor, St. Louis, MO
- Jessica-Anne Chelbda, Certified Pharmacy Technician Supervisor, Providence, RI
- Brad Van Egdom, Compounding Pharmacy Technician, Lincoln, NE
- Constantine (Gus) Vergidis, Pharmacy Director, New York, NY
OCH: Tell us about how you chose to begin your career in pharmacy and how you came to work in home infusion pharmacy?
JC: Prior to working for OCH, I worked for a long-term care facility where we would bubble pack medications. We also had an IV room which is where my compounding journey started. It was very different than what we compound here. The process was more simplistic, comprised mainly of syringes and easy bags of medication. When I started at OCH, I was introduced to all kinds of administration methods that I had never seen before because home care is very different than in a long-term care facility where someone is taking care of you. In that environment, I was dealing mostly with nurses who would infuse the medication for the patient. I believe home infusion is where I would like to settle in my career, it’s by far my favorite pharmacy endeavor that I’ve come across in my ten years of experience.
JB: I began my career as a pharmacy technician in a hospital. I worked at a couple of different hospitals and a former colleague of mine called me about an opening at OCH. I wasn’t looking for a job at the time, but it seemed like an interesting opportunity. I really like working in both the cleanroom and in the hospital. I had never heard of a home infusion pharmacy before but it was a great opportunity and I’m glad I took it.
CV: I began my pharmacy career in home infusion. I actually began my career as a pharmacy intern at Rite-Aid but accepted my first role at Option Care Health within the first year after obtaining my license as a staff pharmacist. Pharmacy school is a long commitment and retail pharmacy doesn’t lend itself to using all of the education I received when becoming a Doctor of Pharmacy. In retail, you only get to see one part of the patient’s picture and with home infusion, you get to see the entire picture of the patient’s health journey. So you’re able to track their progress, ensure that therapy is working, and help them transition off of service because they’ve gotten better.
BV: I’m the one who’s making the actual medication so there’s a lot on my shoulders. I have to make sure I’m making the product accurately and safely. I’m thinking of the patients when I’m doing this –what if it was my mom or dad, grandma, or grandpa?– I’d want it to be as perfect and safe as possible. I try to be very detailed and ensure there are no issues or problems when compounding every drug.
OCH: What made you decide to become a pharmacy technician/pharmacist?
JC: About ten years ago I was going to nursing school, but then life happened. My plans changed and I was doing some research on different fields in healthcare that I would enjoy. I was looking for something that would be hands-on but would require less face-to-face time with patients. I looked into a pharmacy technician training program and attended Lincoln Technical Institute in Lincoln, RI. That gave me the boost I needed to see that there were very different types of pharmacy roles across the board. It’s more than just a retail pharmacy where you would go pick up your medication – that’s not the only option you have as a pharmacy technician to find work. It seemed to me that there were a lot of different options and that I would be able to navigate my way through those options as I became more experienced until I found something I truly had a passion for.
JB: I was thinking about going to pharmacy school but was concerned with the time commitment and wasn’t sure I’d enjoy it. I started at my community college and decided to transfer in my first semester to pharmacy technician studies instead.
CV: The choice to become a pharmacist was easy. I’ve always wanted to help people, especially the sick and needy. I originally wanted to be a doctor or a lawyer but landed on pharmacy because I’m still able to impact the patient. I was also intrigued by the pharmacy growing up and that transitioned into my career later in life.
BV: I actually started my career in retail and I was asked if I’d want to move into pharmacy which wasn’t something I originally thought I’d be into. I didn’t really have any experience before, but I was looking for something new. Whenever I have the opportunity to challenge myself and try something new, I tend to go after it. So that’s what I did and I ended up really liking it. I ended up looking for something to broaden my horizons and applied here at OCH. I was a little nervous at first because it was an entirely new area of pharmacy but I’ve loved it ever since. Every day is different and it’s more varied than a retail pharmacy. I just really like being here.
OCH: How do you deliver hope to our patients?
JC: I think one of my favorite parts about working with Option Care Health is seeing the patient progress through the compounding process. We compound a lot of pediatric total parenteral nutrition (TPN) at our branch and when I first came to this branch, we had a newborn who needed TPN seven days a week. The newborn’s mother was dealing with high stress and anxiety, and now, it’s been probably two years since the patient started on service with us, and they only need TPN three days a week. Seeing that progress throughout the years is really rewarding. To see someone get better, from somebody who needed TPN seven days a week to sustain their life, to someone who can get their nutrition from a source other than a TPN bag, by eating regular foods and drinking regular drinks, is very rewarding. Watching the required doses drop from seven to three and hearing the confidence in the parents as they become familiar with how to take care of their sick child is just so rewarding.
JB: When we’re making the drugs, we see patient names week after week. We don’t really get to know the patients but we do get to know their names. If we notice we haven’t seen a patient in a couple of weeks, we’ll ask about what’s going on. It’s neat to see pediatric patients get off of services because they’ve improved or they had a transplant and no longer need our services. It’s nice to know that we played a part in them getting better and we made safe medication for them and made a difference in their care.
CV: Delivering hope has always been top-of-mind for myself and the other pharmacists I work with. Providing hope is letting a patient know where they currently stand but also reassuring them that OCH is planning for them to get better and sharing what that looks like. We are delivering the medication for these patients, providing a high standard of care, and making sure they’re receiving appropriate treatment while ensuring their safety at home.
BV: I try to put myself in their shoes. The people we are trying to help every day are ill and they may not have a lot of hope in their situation. So if we can make things easier for them and provide the medication they need on time, they don’t have to worry about that and can count on Option Care Health. That’s how we deliver hope.
OCH: What makes being a pharmacy technician/pharmacist at Option Care Health special?
JC: My favorite part is TPN. I’m able to see the progress in our patients and know that I’m personally impacting their overall health. One of the things I’ve recently had the pleasure of doing is working really closely with our Area Clinical Director (ACD), Craig. All of OCH went through the ACHC accreditation surveys and Craig has been a great resource. He always listens to the technicians, truly takes into consideration any suggestions we may have, best practices, streamlining processes, etc. I’ve been working with him on updating some of the forms that are used in the OCH pharmacy and I have great pride in working with him as our ACD in the Northeast.
JB: There’s a lot of trust between the pharmacist and the pharmacy technician. They oversee our work to ensure it’s accurate, but we are the experts when it comes to compounding the medication. We know the proper way to hold a syringe, we know what typical doses are and we know how to reconstitute meds. If we notice something is unusual, we go to the pharmacist and let them know before moving forward because of our expertise in making IVs.
CV: I have the best leadership at OCH. I can reach out to them for guidance or assistance whenever I need to ensure our branch has everything we need. That great leadership is what makes us special because they truly care about us and always ensure that we have everything to provide extraordinary care for our patients. That’s what really sets us apart.
BV: The different opportunities I have here makes a real difference. I feel like we all mean something to the company and I really appreciate that.
OCH: Tell me about working in a pharmacy setting during the pandemic?
JC: When the pandemic first hit, there was a lot of uncertainty throughout the country. Working in a sterile environment, it honestly became scary. One of the great things OCH did is that they started making sure that each facility was environmentally testing their room more frequently to ensure that our cleaning procedures were working effectively. This way, we ensured that we had removed the possibility of creating any room for additional bacteria to grow. At first, things were quite nerve-wracking but seeing that we’ve been environmentally testing our rooms with no positive cultures on any of these tests really goes to show how thoroughly the technicians pay attention to what they’re doing, and that they’re being extra cautious to ensure everything is sterile. The extra precautions that OCH has put into effect have eased a lot of that worry I had before.
JB: We were very clean before and now we’re cleaning even more. I didn’t even know that was possible! It was really nice to know that I would still have my job. When so many people were uncertain if they would be let go or if they could count on their paycheck, I was thankful to know I had one every week. It was a huge relief that with everything else to worry about, I still had a steady job. We actually received a thank you note from a mom who was worried about how her child would receive our medication and the fact that we took the stress off of her shoulders just felt so good. We were proud to be able to provide the proper patient care throughout all of the uncertainty.
CV: COVID-19 obviously had a huge impact on the world and especially New York City. Being in this area during the pandemic has really changed healthcare, our perspectives on what remains consistent and any questions of what’s to come. We have enacted policies and procedures to keep our team members safe at all times: practicing social distancing and wearing masks to keep ourselves and families safe. Being in the epicenter has really led us to work better together because we’ve realized that we’re coming into work to help people and we’ve come together to support the needs of others throughout the pandemic. I feel fortunate to work on this team in New York and to provide care for our patients every day.
BV: I am really proud of how OCH handled the pandemic. As soon as we had an idea that this was going to be a pretty big deal, we began stocking up on things we’d need to use every day. We began working on updating policies and procedures to not only keep employees safe but patients as well. Option Care Health’s leadership did such a great job preparing and handling the pandemic because it has had little to no impact on my personal life.
OCH: Do you have plans to celebrate Pharmacy Week?
JC: I was thinking here at the CMC we could maybe coordinate our outfits or something fun and out-of-the-box to show we’re united and stand out as a team. We truly enjoy what we do to keep our patients healthy and safe.
JB: Yes, we’re going to paste pictures of the pharmacy staff around the office with their face on a superhero’s body and see how many of our team members can find because we are superheroes and want to recognize our team members as such.
CV: In honor of this monumental year we’ve had, we’re celebrating it as Essential Worker Day because we’ve all played a major role. Obviously, the pharmacists and pharmacy technicians will stand out, but we’re going to recognize the entire branch. Our essential workers came in every day, never skipped a beat to deliver hope for our patients, and made sure we took the proper precautions to keep moving forward throughout this unprecedented time.
BV: I think we’re planning to have a nice lunch with the team. It’s been a little more stressful with everything that’s going on but it’s nice to have a moment to sit back, relax, and just celebrate ourselves.
OCH: What does Pharmacy Strong mean to you?
JC: Being Pharmacy Strong is not an individual thing, a lot of teamwork goes into what we do day in and day out. Including pharmacists, we have to work together every day to ensure that we are doing everything appropriately for our patients’ safety. The teamwork behind the pharmacy is what being “Pharmacy Strong” means to me. We really love what we do here at OCH and with so many moving parts, we all need to work together to make sure our patients have a positive experience.
CV: To me, being “Pharmacy Strong” means that we all work collaboratively as one team with one goal: patients come first. We come together, collaborate, and work for our patients as a team to ensure the best care for our patients.
BV: I think that as a group, we are all strong individuals. When you work in the pharmacy, you could have a lot coming at you from all different directions and the team is outstanding. I can trust everybody and I know we all come in every day and give 100%. There can be a lot of weight on our shoulders but we all jump in to help out and make sure the patient is cared for at the end of the day.
OCH: Do you have any final thoughts to share?
JC: Working for OCH overall, I feel like there is a lot of room for growth. In general, there is a lot of room for growth in pharmacy with a lot of different roles that you can encounter as a technician. Just here at OCH, we have warehouse technicians, pump management technicians, clinical technicians who are contacting patients, and compounding technicians. There are just so many opportunities for a pharmacy technician to perform at OCH and in pharmacy in general. When you find the right one, it’s just so rewarding and there’s no limit to your growth within pharmacy itself.
CV: Passionate people make up this company and we are truly dedicated to providing extraordinary care to all of our patients. We are all here to give the best of ourselves to care for our patients every day and I believe that’s representative of our entire organization.
BV: I think the biggest thing I want to say is that when you’re looking at OCH as a company and potential place to work, it can be intimidating for both pharmacists and pharmacy technicians because it’s unlike anywhere they’ve worked previously. It’s something different every day. You can walk in the door and be proud of where you work and love your job. Take the chance, it’s worth it.

Testimonials
National Nurses Week is celebrated each year beginning on May 6 and ending on May 12, Florence Nightengale’s birthday, since 1990. The nurses at Option Care Health deliver hope every day through the extraordinary care they provide our patients. We realized that what makes our nurses so special is that they’re actually superheroes in scrubs.
We took a moment to learn more from four of our nurses on the front lines of patient care every day:
- Kerrie Hollifield, Regional Nurse Manager in Norfolk, VA
- Eileen Atwood, Clinical Care Transition Specialist in Austin, TX
- Crystal Griffin, Infusion Nurse in New York City
- Matt Battson, infusion Nurse in Cincinnati, OH
The following interview highlights just a small fraction of the extraordinary men and women here at Option Care Health.
OCH: When did you know you wanted to be a nurse?
KH: I think I was about 16 years old; I’m from a small town in Michigan and had multiple trips to the ER so I really got to know the ER nurse, Jonie. I told my mom that’s what I wanted to do – become a nurse.
EA: I knew I wanted to be a nurse when I was a little kid, I don’t remember the age. I was in elementary school, probably third or fourth grade. I knew I wanted to work in healthcare and the nurse was the practical choice for me. I always wanted to help people and being a nurse was just what I’ve always wanted to do.
CG: For me, I have always been interested in healthcare and my journey brought me to nursing. Now, I can’t imagine doing anything else.
MB: When I was in high school I was going to join the military in healthcare. Plans changed and that didn’t happen but the journey really came full circle when my daughter was diagnosed with liver cancer when she was a year and a half. Going through that process, interacting with the doctors and nurses that helped take care of her, us as a family, helped me rediscover my passion for nursing, and that was it.
OCH: What does your career as a nurse look like – graduation to first job to infusion?
KH: I began my career with three nursing jobs: two home healthcare agencies and in a hospital in Detroit. When I went to nursing school we didn’t get experience putting in IVs and an LPN asked me to go out and draw blood on a patient. After I successfully collected the samples, I realized that was what I wanted to do so I started doing the IVs in the hospital before transitioning into infusion nursing and eventually to my current role where I serve as an IV Nurse Manager..
EA: I began my career as a NICU nurse before transitioning into field infusion nursing for pediatric patients and cardiovascular home care. I came to Option Care Health in a nurse liaison role helping patients transition from the hospital to their home.
CG: I’ve always been into some form of healthcare. I started my career really as a dancer and a choreographer really focusing on mental health. That turned into a job with special needs children and then I began working with elderly, special needs adults before I became med certified and finally received my LPN.
MB: I actually began my career as an aide in a nursing home in high school before I became a chef and began working down the path of opening my own restaurant. Once everything happened with my daughter though, I realized being a nurse was what I was meant to be. Therefore, I put myself through nursing school and am working on my bachelor’s degree today.
OCH: How long have you been with OCH? What drew you to OCH and what keeps you here?
KH: I’ve been with Option Care Health for 18 years. I originally started because of the nurse in charge of the business at the time. I respected her so much and decided I’d like to work for her so I joined the company and stayed because of the great people. Here in Norfolk, we’ve worked together for so long, we’re like a family.
EA: I initially came to Option Care Health because of the people – they just loved working here. I love having autonomy out in the field, not working 12-hour shifts but being able to help teach these patients when they have no idea what they’re doing or how they can do it at home, it’s just a rewarding aspect of nursing.
CG: I’ve been with Option Care Health for about four years, ever since I’d heard how rewarding infusion nursing was as a career. I had been doing dialysis but I was looking for something that would use both my technical skills and my bedside manner. This company has been so good to me; the people are extremely supportive and always make sure I have everything I need to do my job safely. I don’t feel like I’m working, I love it that much.
MB: I’ve been with OCH for about five years and I think I stay because of my manager and the people I work with. I also love my patients, I get to know them on a deeper, personal level and I’m able to help them because of the amount of time I’m able to spend with them.
OCH: In your opinion, what makes nursing at OCH special?
KH: Besides many of us being certified infusion nurses, we’re allowed to take the time we need with the patients to make sure they are comfortable. We’re able to do the teaching that allows them to be comfortable in their home or an Option Care Health Infusion Suite (AIS) with whatever therapy they are receiving.
EA: Everyone has the same goal. We work together as a team and we just want the same things no matter what area of the business you’re in. It’s all about the patient and making sure they’re taken care of – someone always has your back, people are open to ideas and you’re not alone out there.
CG: The term above and beyond exemplifies the nurses here. Every nurse will always go above and beyond to serve the needs of the patient and help the organization move forward. There’s nothing we wouldn’t do for our patients. I have an example, last week a nurse, Kim, came to New York City from Buffalo during height of COVID with bells and whistles on to help us for the week. That’s the kind of thing that makes OCH different.
MB: This is a unique environment that we all work independently, we’re not working side by side with our coworkers. However, I’ve never met any of our nurses that wouldn’t be willing to go the extra mile to help to provide the extraordinary care our patients deserve. That is truly unique to OCH and it’s very special to find people who are truly willing to help no matter what.
OCH: How do you plan to celebrate yourself during national nurses week?
KH: I haven’t really given it much thought. For me, what I do for peace and quiet is to go fishing.
EA: I don’t usually do anything because it’s my job, it’s all I’ve known. I just carry on and make sure the patients are taken care of, that’s my celebration. I don’t need recognition for something I enjoy doing, I truly get that when I’m caring for patients every day.
CG: I’ll probably do a Zoom with my family without interruptions. It may not sound like a lot but I just lost my grandmother over the weekend and taking time with my family that’s filled with joy amid all the negativity, it just fuels me. Even the fact that we’re social distancing and visiting in that way, it makes a big difference for me.
MB: Honestly, I don’t need any accolades or celebration, I truly enjoy what I do and it feels like it’s what I was meant to do. Being able to provide care for my patients is the only celebration I need.
OCH: What does it mean to you, to be providing extraordinary care during an unprecedented time like the one we’re currently in?
KH: I think for us, we have moved many of our patients into our infusion centers. I’ve been able to communicate with our patients and explain why coming to an AIS is lowering risk because of our cleaning procedures between patients. We are also able to lower the risk of exposure by not going into multiple houses to provide care. It’s the first time we’ve ever had to do this but it has been successful It’s working so far and we’re maintaining the health of our patients with their care at the forefront of what we do.
EA: I’m still able to get into the hospitals to teach but the biggest thing is not portraying fear to anyone. To me, the challenge is bridging the gap for the family and the patient. I had a patient the other day who was in the hospital for 11 days, alone. I had to help the family and the patient feel connected with their care, navigate the discharge process, manage the patient’s care after they returned home and help them believe that they successfully provide that care in their home.
CG: I build my happiness around my intentions. My intention is that every patient we care for comes away with an experience that was the same or better before COVID-19. Of course we are implementing safety measures that are different than before but I hope the quality of their care is being maintained or even better than before. I want Option Care Health to be known as a company that cares right now and throughout everything that happens after today.
OCH: What advice you have for people wanting to celebrate everything front line workers are doing during this pandemic?
KH: I enjoy the simple thank you’s. I am glad I’m a nurse, the most trusted profession; I just think the simple thank you’s go a really long way.
EA: What means the most to me is just saying thank you, you’ve made a difference and thank you. That’s all I need.
CG: This is a funny thing because when I got into nursing, I realized that my “applause” comes from within. When a patient is discharged, that is all I need to hear – Thank you for all you’ve done.
MB: I suppose, just a simple thank you. Honestly, that’s more than enough; I do what I do because I love what I do.
Globally, the nursing profession is celebrating a milestone in 2020, as the World Health Organization declares it the International Year of the Nurse and Midwife in honor of the 200th anniversary of the birth of Florence Nightingale.
Thank you for all you do for patients across the country today and every day. Happy Nurses Week.

Testimonials
Easing patient worries about therapy costs
Helping ease patients’ financial stress is why Priscilla O’Quinn loves her job. As an Option Care patient benefit navigator, she is a master at unearthing resources to ensure they can afford their medication. In fact, in one five-month period alone, Priscilla secured over $1 million in copay assistance for Option Care home and Ambulatory Infusion Suite patients from manufacturer copay assistance plans and foundation related grant dollars.[*]Savings due to the financial assistance programs referenced in this article may not be available or applicable for all patients.
“I find a way to help people in some way, shape or form,” said Priscilla. “It makes my heart very happy.”
Financial assistance can make the difference
She remembers the man with hemophilia who required life-saving IV Factor VIII protein therapy to prevent excessive bleeding. He couldn’t afford to keep his Medicare supplemental insurance and could only manage to pay a small portion of his bill each month, putting him into growing debt. Priscilla determined he qualified for a hemophilia financial assistance program and enrolled him. The program paid his bill in full and reimburses his insurance premiums.
“When I told him, he said ‘You’re an angel!” Priscilla recalls.
Priscilla constantly monitors foundations and other financial programs to assess when slots for assistance become available and uses a variety of other avenues to help patients receive monetary support.
For example, one patient on Medicare was prescribed subcutaneous immunoglobulin (SCIG) to treat her autoimmune deficiency. She was prepared to tell her doctor she just couldn’t afford the treatment – but Priscilla found a way to help her. Because the woman also had lupus, Priscilla connected her to a foundation that covers almost all of her copay for intravenous IG (IVIG) and assists in paying for her other medications too. She gladly switched from SCIG to IVIG and now pays a fraction of the cost.
Always on the lookout for opportunities
While manufacturers often have financial assistance programs, patients can’t benefit from them if they have government insurance (such as Medicare or Medicaid). So, Priscilla reaches out to foundations and other support plans and – as for the patient with lupus – evaluates if aid is available due to their other conditions. Sometimes changing the method of therapy or medication makes the difference.
Priscilla embodies Option Care’s commitment to providing patients with high quality care and support. She frequently gets calls from grateful patients looking for advice about how to pay for an expensive prescription unrelated to their infusion therapy and she always tries to help. “Money is a big concern and often stops people with serious conditions from adhering to their treatment, so we find a way to solve that problem for all of our patients,” she said. “It means so much when they have somebody who cares for them, and they can really hear it in your voice.”

Testimonials
After overcoming ovarian cancer in 1995, retired nurse Lydia Zwilling found herself facing an arduous battle to reclaim her health. Nearly a quarter million women are diagnosed with ovarian cancer every year and for most, treatment goes according to plan. Unfortunately, some like Lydia, experience complications that last a lifetime.
While radiation therapy may have saved Lydia’s life, it also burned her small intestine and contributed to complications that ultimately caused her kidneys to fail. She had to be put on dialysis for two years before she was able to receive a kidney transplant in 2006.
Doctors also had to remove the burned portion of her small intestine, leaving her with just three functioning feet of her bowel. Diagnosed with short bowel syndrome (SBS), Lydia started to experience dramatic weight loss because her body could no longer absorb adequate nutrition. At 72 pounds, she was emaciated and unable to regain any weight. She became home-bound.
“I felt deeply frustrated,” Lydia said. “After beating a life-threatening cancer, I still had no strength or energy. I decided it was time to take some action to see what could make me better.”
In 2006, Lydia was introduced to Option Care by her attending physician and put on total parenteral nutrition (TPN), which gives her the nutrition she needs through intravenous delivery.
“TPN made an immediate difference in my overall health,” Lydia said. “I finally started to feel like myself again.”
Lydia and her husband are registered nurses so they are able to handle her TPN treatments and labs from home, self-infusing five days a week for nine hours at night. Lydia works closely with her care team at Option Care to receive additional antibiotics when she needs them. They also coordinate directly with her physicians to communicate any changes in her treatment.
“After many years with Option Care as my infusion provider, I’ve developed a close relationship with my care team and we’ve gotten to know each other on a personal level,” Lydia said. “You can tell that they care about what is going on with me and not just my medical health. I have complete confidence in their abilities to provide me with the best care possible.”
As a grateful cancer survivor, Lydia is thriving thanks to TPN. She credits her involvement with Option Care as enabling her to regain a near normal life. She is now able to visit her grandchildren who live six and a half hours away as well as escape the cold Minnesota winters for vacations in Florida and Arizona. Option Care supports Lydia by working with her to ensure she has access to necessary medications while she’s traveling.
“I can get out and get back a little bit of my life that I had before,” Lydia said. “It’s important to spend your energy on trying to get yourself better. Option Care home infusion helps me do that.”
