Featured Stories
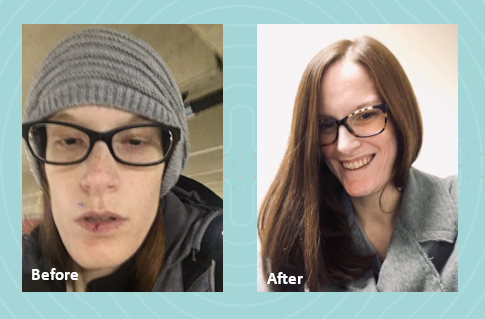
In 2022, I graduated from nursing school with dreams of starting my career as a nurse. However, life had other plans. I was diagnosed with gastroparesis, a condition that made it impossible for me to work and pursue my passion. As my condition worsened, I had to put my career on hold to focus on my health.
 Initially, my local clinicians recommended jejunal feedings, which I tolerated well at first. However, after my J-tube surgery, my condition began to deteriorate, and eventually I became severely malnourished. I was surviving on a mere 500 calories a day, leaving me too weak to perform even the simplest tasks. My mom had to help me with everything, including bathing. Living in a two-story home became a daily struggle, as I had to crawl up the stairs, feeling my body slowly giving up.
Initially, my local clinicians recommended jejunal feedings, which I tolerated well at first. However, after my J-tube surgery, my condition began to deteriorate, and eventually I became severely malnourished. I was surviving on a mere 500 calories a day, leaving me too weak to perform even the simplest tasks. My mom had to help me with everything, including bathing. Living in a two-story home became a daily struggle, as I had to crawl up the stairs, feeling my body slowly giving up.
My local registered dietitian recommended Parenteral Nutrition (PN) and sent the order. We were then referred to Option Care Health (OPCH). I was scared to start PN, but my OPCH dietitian reassured me, saying, “Just because you’re on PN doesn’t mean your life is over. The goal is to give you back more of your life than before.” Her words stuck with me, offering hope during a difficult time.
Due to my blood sugar issues, I’m on 23-hour PN feeds and carry a backpack that has become a part of me. Despite these challenges, my OPCH team has been incredible. My registered dietitian and pharmacist have truly been lifesavers. I continue to speak with my OPCH registered dietitian weekly because she genuinely cares about my well-being and supports me through every step of my journey.
Thanks to the unwavering support of my Option Care Health team and my local registered dietitian, I am back to work and feeling so much better. I wholeheartedly recommend Option Care Health to anyone in need. They have played a crucial role in my recovery, and I am forever grateful for their dedication and care.

Featured Stories
Gastroparesis refers to a delay in emptying stomach contents. Symptoms often include feeling full after eating a meal, or even a small amount of food, as well as nausea, vomiting, bloating or abdominal pain. The causes of gastroparesis may include diabetes mellitus, complications after surgery, kidney disease, certain medications, thyroid disorders, cancer, among others.
The following tips are intended to reduce symptoms and help maintain adequate nutrition.
|
Mealtime
|
||
|
Foods
|
|
|
Fluids
- Stay hydrated. Most adults need 6-10 cups of water per day. Sip slowly throughout the day.
- Drink fluids with meals, however; be sure not to fill up on liquids
- Avoid carbonated beverages as they can cause bloating
Other
- Avoid alcohol as it can affect stomach emptying
- Foods that are acidic, spicy, or contain caffeine or mint may increase acid reflux
- Keep blood sugars under control if you have diabetes
- Keep a food diary to track your intake and find foods that are best tolerated
- Exercise may increase stomach emptying and reduce symptoms. Walking after meals is suggested.
See below for help in choosing more optimal foods from each food group:
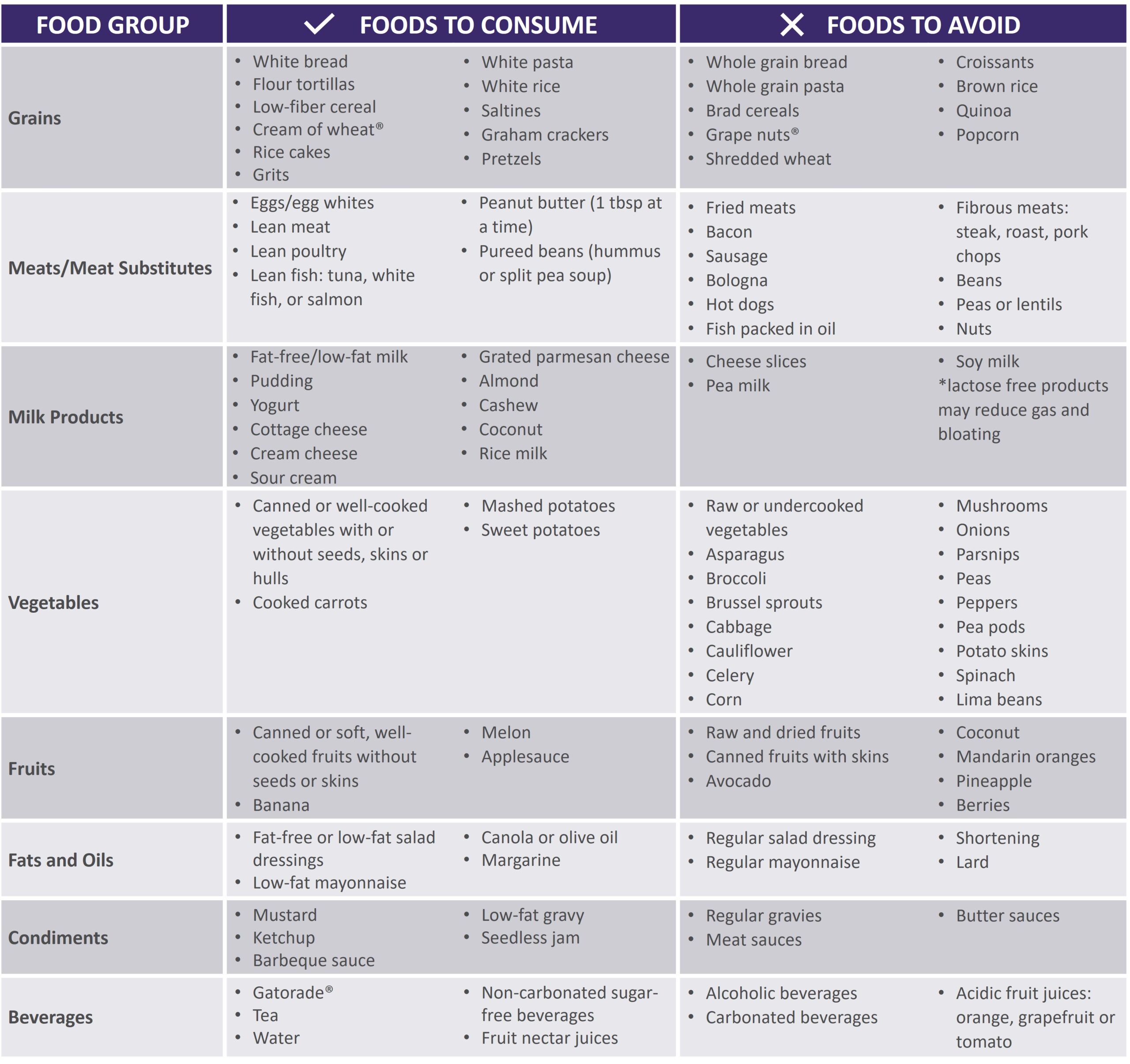 |
|
Gastroparesis Sample Menus |
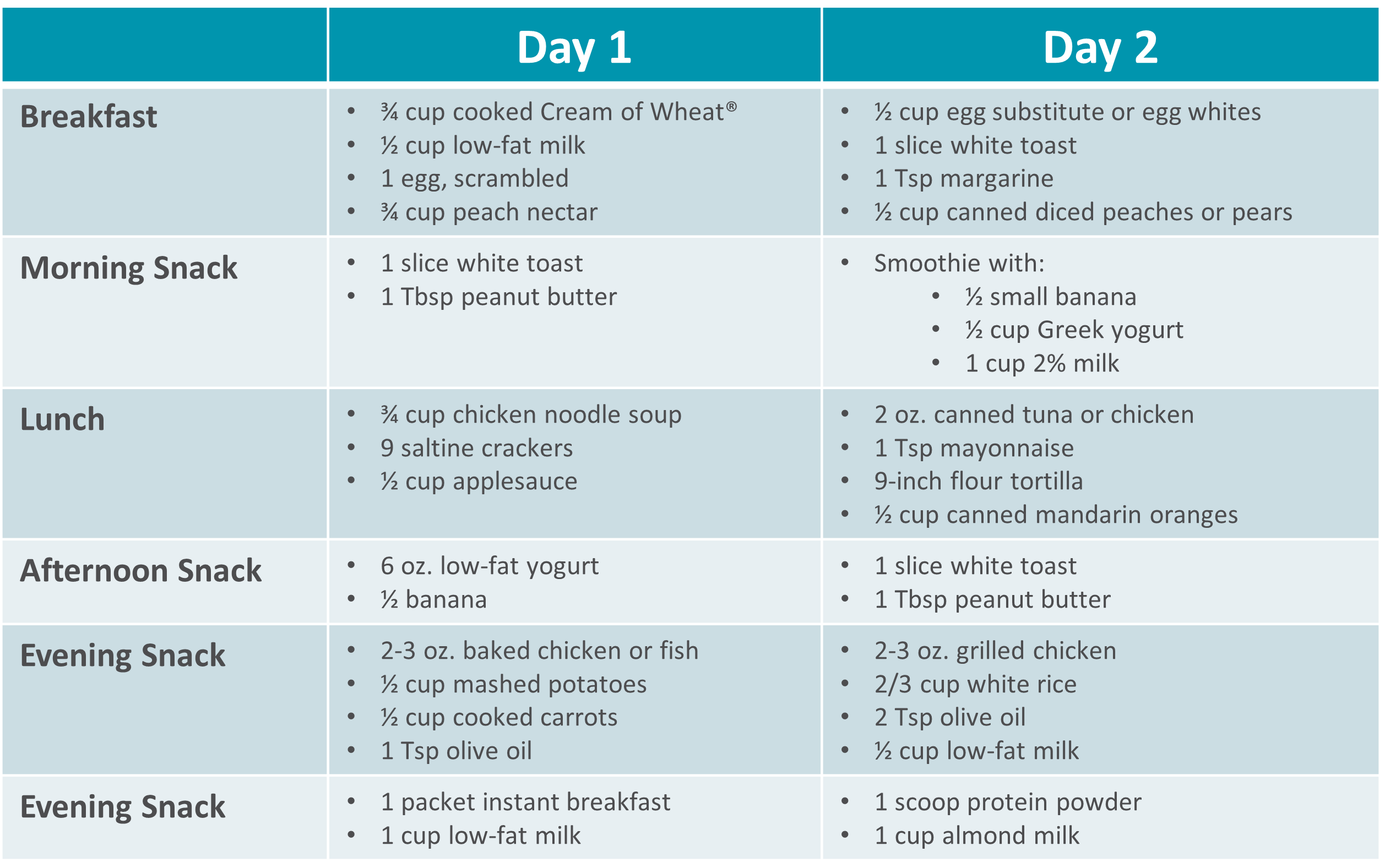 |
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health.
*This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information.

Featured Stories
Short bowel syndrome (SBS), or intestinal failure, is a condition in which your body is unable to absorb enough nutrients from foods and fluids you consume. This can occur after a surgical resection or damage to your intestines. Symptoms and absorption vary by individual based on the amount and health of the remaining intestine. Symptoms of SBS can include diarrhea, dehydration, electrolyte abnormalities, and weight loss.
The following tips are intended to maximize absorption, improve your nutritional status and reduce dependence on parenteral nutrition.
- Mealtime
- Eat small, frequent meals (6-8 per day)
- Foods
- Eat protein at all meals: eggs, creamy peanut butter, chicken, fish, beef, tofu
- Choose complex carbohydrates such as bread, pasta, rice, and potatoes
- Limit raw vegetables to small amounts
- Avoid fruits with skin or edible seeds
- Limit raw fruits to very small portion twice a day
- Increase your soluble fiber to thicken output with foods such as bananas, applesauce, rice, oatmeal or use of soluble fiber supplements
- Avoid high fat foods such as fried foods if your colon is intact
- Use caution with dairy products – lactose intolerance is common with SBS
- Avoid concentrated sweets such as candy, desserts, and juice
- Avoid foods artificially sweetened with sorbitol or mannitol (Splenda® is okay)
- Fluids
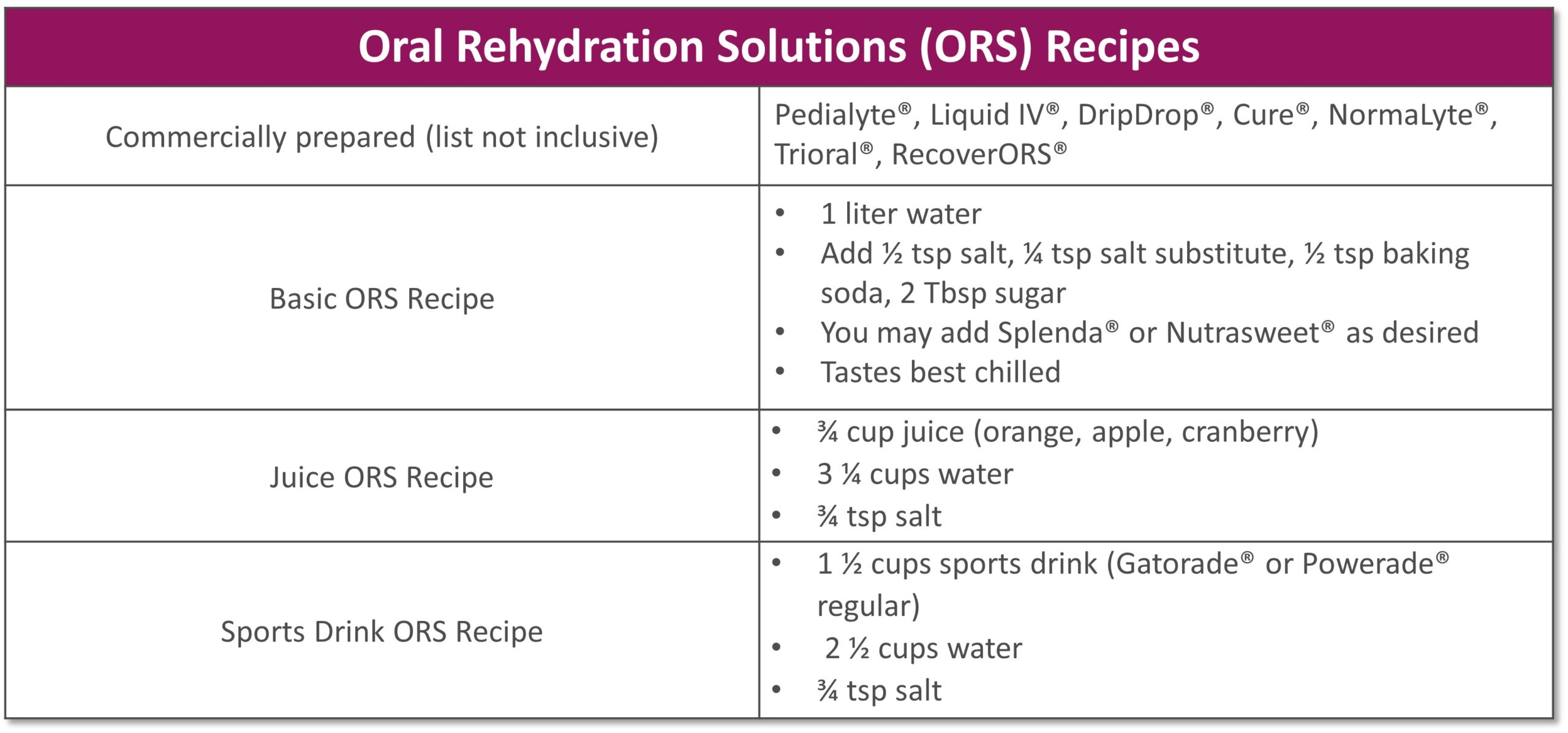
- Drink isotonic fluids (with electrolytes), ideally oral rehydration solutions (see recipes below)
- Do not drink fluids with meals as it increases how quickly food passes through
- Limit to 4 oz. fluid during your meal to allow your food to be best absorbed
- Drink ½ hour before or 2 hours after eating
- If you do not have your colon, your fluid losses will be higher
- Other
- If prescribed by your doctor, take antidiarrheal medication ½ hour before meals
- Salty foods such as pretzels or soups are usually well tolerated and help absorb fluid
- Avoid caffeine and alcohol
See below for help in choosing more optimal foods from each food group:
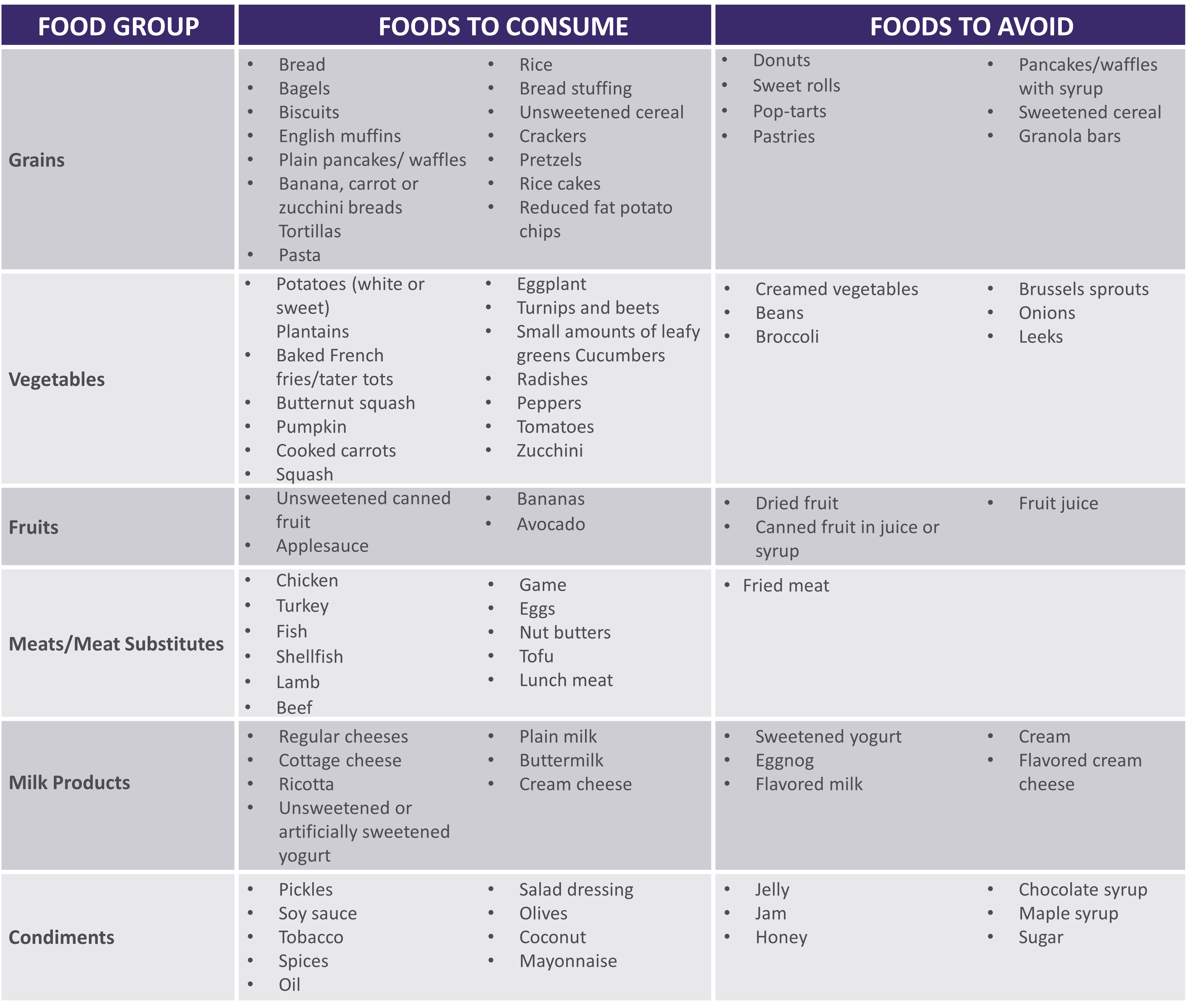 |
|
|
|
**For homemade ORS, discard after 24 hours if not consumed **Visit for more recipes: https://optioncarehealth.com/patients/resources/sbs-friendly-recipes |
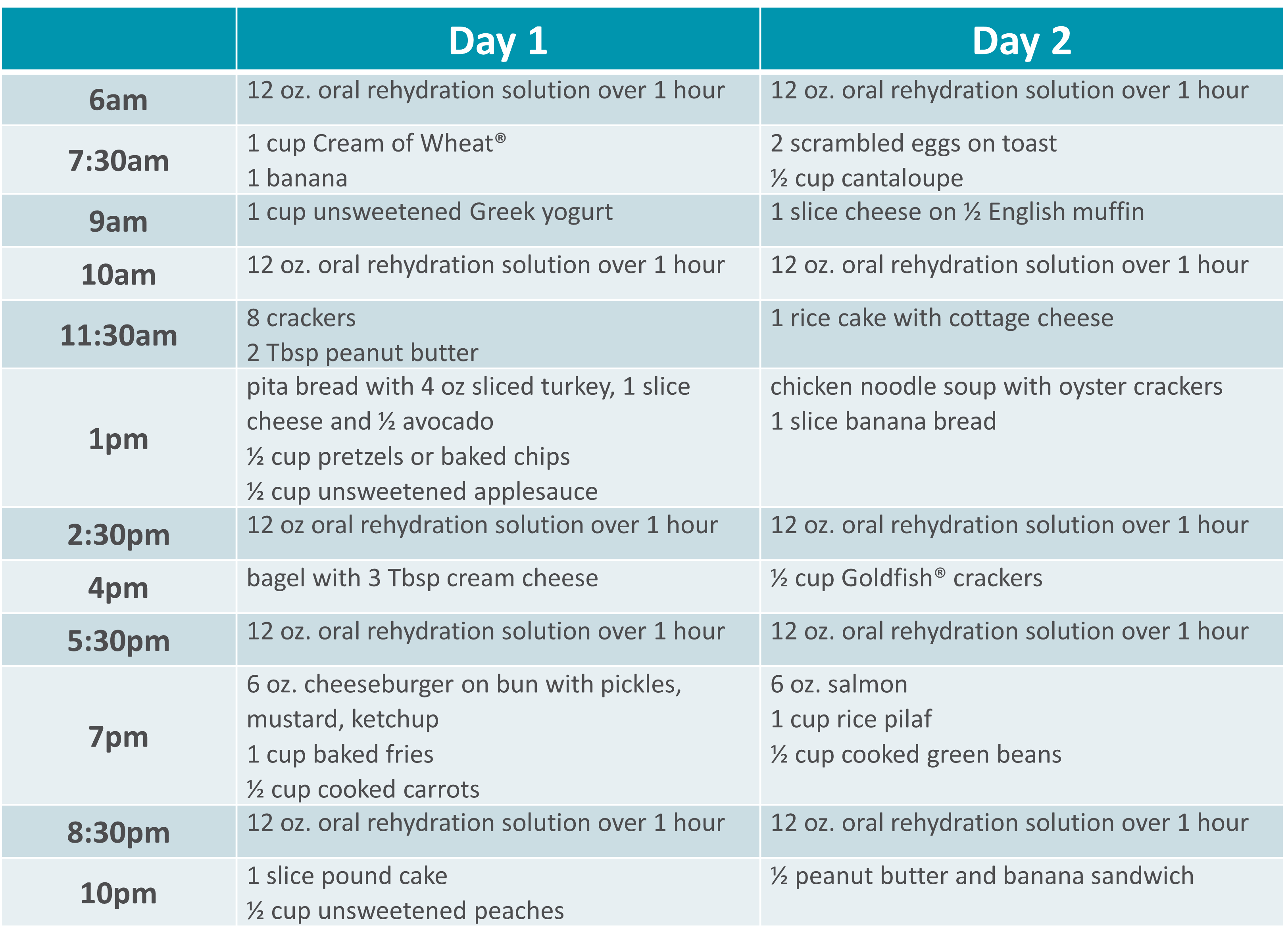
SBS Sample Menu |
 |
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health.
*This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information.

Featured Stories
Gillian was just 11 years old when she began treatment for multiple complex chronic illnesses. As a teenager, she was diagnosed with gastrointestinal (GI) motility disorder and gastroparesis, which led to long-term, severe malnutrition.
“It was really hard missing out on so many activities growing up. I was prescribed various medications and tube feedings, but nothing helped long term. By early adulthood my symptoms worsened so I had to withdraw from college and take an extended medical leave from my job,” she said.
From 2015 to 2018, Gillian’s health progressively declined. “I was on tube feeds and other intravenous (IV) medications at the time. I began losing weight again, my neurological function was declining and I couldn’t speak or walk.” As Gillian’s health continued to decline, she found the strength to advocate for herself and build upon her excellent team of healthcare providers.
Gillian was put on total parenteral nutrition (TPN) in 2018, managed by Option Care Health. “This was my turning point. Today my labs are perfect and my cognitive function is back to normal. My weight has stabilized and I’m back to living life. I owe so much of my progress to my Option Care Health team.” Gillian continued, “My registered dietitian (RD) is amazing. During the initial COVID outbreak, I was struggling with my health and I couldn’t reach my doctors, but my Option Care Health RD was there every time I reached out. I got the help I needed and I owe it all to her.”
She claims that her Option Care Health team including her pharmacist and pharmacy technician go above and beyond expectation. “Other companies and even providers don’t always focus on how the patient needs to be living their best quality of life during treatment. My team at Option Care Health set up my deliveries in the evening to accommodate my work schedule. They also deliver them upstairs to me because I’m unable to carry them. My pharmacist and tech were so helpful this summer. They were able to find a way for me to go on vacation by switching around my infusions and supplies. Thanks to their help, I was able to go on my first trip since 2015! They are really focused on me as a person, not just a patient.”
Her message to her Option Care Health team is one of gratitude, “I just want them all to know how appreciative I am. They have and continue to be a key part of my recovery and I couldn’t be more grateful.” Gillian is thriving and living her best quality of life. She’s working, volunteering and spending as much time as possible with family and friends.
Learn more about malnutrition and join us in spreading awareness this ASPEN Malnutrition Awareness Week*, September 19th-23rd: ASPENMAW22
*Malnutrition Awareness Week™ is a mark of the American Society for Parenteral and Enteral Nutrition (ASPEN). Used with permission from ASPEN.

Featured Stories
Four years ago, Sherry Hambly, 56, developed a painful rash, that constantly felt as if she had a terrible sunburn. Her skin burned every time she washed her hands or took a shower and her muscles were weak. After a long journey searching for answers, she was diagnosed with dermatomyositis, an autoimmune disorder. She’s now receiving intravenous immunoglobulin (IVIG) at the Option Care Health Infusion Suite in Troy, Mich., and is grateful to have her life back.
Prior to finding the right diagnosis and treatment, Sherry was so uncomfortable she had to take pain medicine daily and could barely perform her job as an accountant, due to weakness. She didn’t sleep well and was too exhausted to relish the things that brought her joy, including playing with her grandchildren, golfing, bowling and doing yoga.
“I love the employees at the Troy infusion suite because I never have to lift a finger – they take care of everything and made sure my care plan was personalized for me,” said Sherry, of Rochester Hills, Mich.
Early on, she was taking hydroxychloroquine, a high dose of steroids and an anti-rejection drug. Her original IVIG prescription involved four-hour IVIG infusions three days in a row once a month, but by the end of the month the benefits wore off and she didn’t have the energy to go to the office. The Option Care Health team worked with Sherry, her doctor and pharmacist to devise a care plan that worked best for her and she now receives the infusions two days a week every other week.
“It’s made all the difference in the world,” she said. “I no longer take any pain pills and am completely off all the steroids I relied on to keep me moving, because my IVIG treatment is helping so dramatically.”
She lives with her husband, son and two grandchildren. Now that she has her energy back, she’s able to assist her 11-year-old grandson with his home schooling and watch her 16-month old granddaughter. She’s back to golfing and doing yoga and can perform her job to her fullest potential.
“I really like the infusion suite – it’s nice being in your own little space during COVID-19 – the room has windows, comfortable chairs and a kitchen where I can warm up my coffee. It’s quiet and I can even work while I’m there,” she said. “The staff is always going above and beyond to make sure we’re safe and comfortable.”

Featured Stories
Frequently ill with pneumonia, bronchitis and other serious infections, Cambria Hooven, 35, limited her contact with people and didn’t leave her house much. After finally learning the reason for her near-constant sickness was a weakened immune system due to common variable immune deficiency (CVID), she began receiving intravenous immunoglobulin (IVIG) at home through Option Care Health. She felt free to get out more and socialize, but then the COVID-19 pandemic hit.
Because Cambria was afraid to risk having visitors come to her home, her Option Care Health nurse, Kola devised a plan. He suggested she receive treatments at the Option Care Health Langhorne Infusion Suite where he works, which is a 35-minute drive from her home in Philadelphia.
“I was nervous about it as I hesitate to go anywhere during this pandemic, so he sent me a video of the suite before my first appointment, walking through everything and showing me exactly what doors to enter,” said Cambria, who gets teary eyed at the memory. “Kola has been my nurse for two years and he’s like family to me. I don’t know what I would do without him in my life!”
She now receives her four-hour monthly treatments in a clean and sanitized room, which has its own comfortable lounge chair and large windows. Because she otherwise stays home during the pandemic, she really enjoys going for her monthly infusions. “It’s a little retreat center,” says Cambria.
Cambria is relieved to finally have a diagnosis and receive treatment. For years, she saw one doctor after the next to try to figure out why she was always sick. Eight years ago, she had her appendix removed, got a serious blood infection and spent 33 days in the hospital, unsure if she would survive. Determined to get to the bottom of her problem, she took a leave from her job as a social worker in child welfare to have one test after the other.
She finally saw an immune specialist who diagnosed her condition and prescribed IVIG. As a result, she hasn’t been hospitalized since. Initially, she began self-infusing at home, but wasn’t comfortable with it. Option Care Health recommended a nurse come to her home to provide the infusions and that’s how she met Kola.
Now that she’s receiving treatment, Cambria feels healthier and is able to do her work as a social worker remotely, often from the Langhorne infusion suite.
“I know how to stay safe and the treatment I get at Option Care Health helps so I don’t have to live in fear and isolation. I can get outside safely to hike and backpack,” she said. “It’s great going to the Langhorne suite, which is safe and clean and I have so much respect for the nurses and their families. They’re so considerate.”

Featured Stories
Abbi Tucker’s simple wish is to be a normal teenager and enjoy playing music, but when she was 13, severe migraine headaches and terrible stomach aches, that resulted in a 50-pound weight loss, derailed her hopes for a while. After numerous tests and consultations with doctors she was diagnosed with Crohn’s disease, an inflammatory bowel disease. Her life is back on track now that she receives infusions of therapy treating chronic inflammatory disorders at Option Care Health’s Troy Infusion Suite.
“Once I started getting treatment, my life changed,” says Abbi, now 16, of Marysville, Mich. “I gained the weight back and could finally focus on school and having fun again.”
When Abbi started experiencing severe health issues, she and her family were frightened and she was miserable. Her symptoms caused her to miss at least one day of school a week and she found it difficult to keep up with her studies. She couldn’t hang out with her friends, play or teach piano, and even lost her appetite.
Now with a treatment plan in place, she’s back to her activities, including band practice as a junior drum major, spending time with friends and playing music at her church. Eating is also gratifying, although she stays away from greasy and spicy foods as well as popcorn.
Abbi originally received her one-hour therapy every seven weeks at the hospital. When insurance issues arose necessitating a switch to an infusion company, she and her family selected Option Care Health and couldn’t be happier with their choice.
“I LOVE the nurses there,” she said. “I have a hard time getting my blood going for blood draws, which made them painful. One of my Option Care Health infusion nurses made me a heating pad and I use it every time I get my blood drawn. It’s amazing.”
Antonette, the receptionist at the facility, calls to remind her family about upcoming appointments and the staff knows to look for her dad’s red truck when she gets dropped off. He’s a fireman and paramedic with a medical background, which puts her family at ease.
She likes getting her care at the infusion suite instead of at home because she occasionally has had adverse reactions. She takes Benadryl and a steroid before every treatment, which helps, but she’s comforted to know that Option Care Health nurses are nearby if she starts having issues. She also appreciates the privacy of the suites.
“The staff always makes me feel right at home and that my health is their number one priority,” said Abbi. “Infusion therapy really has been lifechanging and now I can do what a typical 16-year-old would do every day.”

Featured Stories
As the COVID-19 pandemic continues to alter the home-based care industry, changes that agencies were already making to succeed in a value-based care model have taken on a new urgency. Innovative technologies are critical to help prioritize value-based data and seamless transitions to lower-cost care settings.
For both economic and safety reasons, home care plays an increasingly important role in minimizing risk for elderly or otherwise immuno-compromised patients, especially for those who rely on infused drug therapies for chronic, complex conditions. With hospital system capacity spread thin due to the pandemic and elevated concerns about risk of exposure in a health system setting, the imperative for keeping people in the comfort of their own homes is greater than ever.
That is what makes home infusion therapy so appealing.
Home infusion comes with significant benefits, but the industry also faces a new set of challenges due to COVID-19. Adoption of flexible, scalable technology is an important part of the solution to support in-person and virtual operations while building new processes that will chart a course well past the point of the pandemic’s impact.
With its required mix of equipment, complex therapy management and clinical coordination across many health care providers, home infusion creates strain around data tracking and operational efficiencies. To address these challenges, home and alternate site infusion providers need a software platform that is cloud-based and mobile, offers real-time communication and integrates seamlessly with other systems to provide users with a single point of access.
“As the demand for home infusion rises, the need to ensure patient safety and high-quality care will be a key focus,” says Adrian Schauer, founder and CEO of a cloud-based, home health care software provider AlayaCare.
Here are five benefits that cloud-based technology brings to home and alternate site infusion during the pandemic.
Offers easy-to-use technology
For Option Care Health, a partnership with AlayaCare has been just what the doctor ordered. One of the major advantages is the ease of the technology, which was a key selling point for nursing teams accustomed to pen and paper.
“We needed a solution that would be easy to adopt, help us easily shift to a virtual environment and meet the increasing need for data,” says Joan Couden, vice president of nursing for Option Care Health. “The IT match was really important to us. The solution we chose had to fit into the rest of our systems and clinical needs.”
Enhances nurse-pharmacist communication and collaboration
One of the most important relationships for optimizing outcomes in home infusion is between the nurse and the pharmacist. The pharmacist must know everything happening during the care episode, while the nurse must know all of the medications the patient is taking orally as well as what is being compounded and dispensed from the pharmacy.
Previous to its work with AlayaCare, Option Care Health maintained this nurse-pharmacist collaboration through manual processes, which “are always sub-optimal,” Couden says.
Instead, cloud-based technology produces near real-time updates to care plans, moving from the nurse to the pharmacy or the pharmacy to the nurse. Changes to medications or patient response to medications get transferred immediately.
“Now more than ever, post-acute care providers must automate manual business processes to ensure high-quality care, or risk missing out on profitable growth,” Schauer says.
Creates consistent care regardless of setting
In a mobile world, amidst a pandemic and a value-based landscape that rewards care in lower-cost settings, the ability to deliver care in a patient’s home is invaluable, with multiple benefits to both care outcomes and the bottom line.
But the home is not the only location where infusion services are provided. Patients can also receive care in infusion suites. Cloud-based technology offers continuity of care across settings to ensure that the quality of care is the same no matter the setting.
“There are a lot of challenges in a remote, mobile clinical situation. The AlayaCare platform allows for flexible, dynamic adaptation to the way home infusion worked historically and to how it is changing today,” says Brett Michalak, Option Care Health Chief Information Officer. “Everyone can be focused on clinical care for the patient, and not the underlying technology. And that means patient experience and outcomes are highly enabled through this partnership.”
“The technology allows us to focus on providing care in the most efficient way possible,” adds Couden. “We can ensure we are matching the right nurse to the right patient all with a click of a button, helping to minimize travel time and increase patient-facing time.”
Facilitates shift to telehealth
While this technology had great value prior to the COVID-19 pandemic, Option Care Health has seen a boost in its value during the pandemic. Cloud-based technology supports that shift — a shift which is likely to continue to deepen in the coming months.
“The pandemic caused us to look at everything we do differently,” Couden says. “When we started this journey (with AlayaCare), would I have said, ‘Telehealth is something we have to do right now’? I probably would not have. But working in partnership with AlayaCare and our clinical teams, we were able to rapidly and smoothly deploy virtual solutions that really have the ability to change lives for the better, one patient at a time. I believe this is an integral part of how health care will continue to be delivered now and in the future.”
Deploys quickly due to easy integration
One of the top concerns care providers have about new technology systems is workflow. They ask themselves, How long will this take to integrate? The answer from AlayaCare is nearly instantaneous, regardless of what technology a provider already uses.
“AlayaCare allows us to deploy the technology in a rapid manner,” Michalak says. “Competitive platforms don’t provide the integration capabilities, in my opinion, that AlayaCare can provide. The integration of the platform allows for rapid adoption.”
The needs for quick integration and streamlined collaboration are obviously high during COVID-19, but when Option Care went through a merger last year (launching as Option Care Health), the technology from AlayaCare helped the company quickly pivot, too.
“The agile nature of the platform allows us the flexibility to adjust to any evolution in our care environment,” Michalak says. “Whether that’s a merger or a pandemic, we can adapt and deploy the technology optimally to enable our clinicians to focus on care and not on administrative technology. The ease of use and scalability lets our clinicians perform at their highest levels.”
To learn more about how AlayaCare can help your home infusion business, visit AlayaCare.com today.

Featured Stories

Featured Stories
National Nurses Week is celebrated each year beginning on May 6 and ending on May 12, Florence Nightengale’s birthday, since 1990. The nurses at Option Care Health deliver hope every day through the extraordinary care they provide our patients. We realized that what makes our nurses so special is that they’re actually superheroes in scrubs.
We took a moment to learn more from four of our nurses on the front lines of patient care every day:
- Kerrie Hollifield, Regional Nurse Manager in Norfolk, VA
- Eileen Atwood, Clinical Care Transition Specialist in Austin, TX
- Crystal Griffin, Infusion Nurse in New York City
- Matt Battson, infusion Nurse in Cincinnati, OH
The following interview highlights just a small fraction of the extraordinary men and women here at Option Care Health.
OCH: When did you know you wanted to be a nurse?
KH: I think I was about 16 years old; I’m from a small town in Michigan and had multiple trips to the ER so I really got to know the ER nurse, Jonie. I told my mom that’s what I wanted to do – become a nurse.
EA: I knew I wanted to be a nurse when I was a little kid, I don’t remember the age. I was in elementary school, probably third or fourth grade. I knew I wanted to work in healthcare and the nurse was the practical choice for me. I always wanted to help people and being a nurse was just what I’ve always wanted to do.
CG: For me, I have always been interested in healthcare and my journey brought me to nursing. Now, I can’t imagine doing anything else.
MB: When I was in high school I was going to join the military in healthcare. Plans changed and that didn’t happen but the journey really came full circle when my daughter was diagnosed with liver cancer when she was a year and a half. Going through that process, interacting with the doctors and nurses that helped take care of her, us as a family, helped me rediscover my passion for nursing, and that was it.
OCH: What does your career as a nurse look like – graduation to first job to infusion?
KH: I began my career with three nursing jobs: two home healthcare agencies and in a hospital in Detroit. When I went to nursing school we didn’t get experience putting in IVs and an LPN asked me to go out and draw blood on a patient. After I successfully collected the samples, I realized that was what I wanted to do so I started doing the IVs in the hospital before transitioning into infusion nursing and eventually to my current role where I serve as an IV Nurse Manager..
EA: I began my career as a NICU nurse before transitioning into field infusion nursing for pediatric patients and cardiovascular home care. I came to Option Care Health in a nurse liaison role helping patients transition from the hospital to their home.
CG: I’ve always been into some form of healthcare. I started my career really as a dancer and a choreographer really focusing on mental health. That turned into a job with special needs children and then I began working with elderly, special needs adults before I became med certified and finally received my LPN.
MB: I actually began my career as an aide in a nursing home in high school before I became a chef and began working down the path of opening my own restaurant. Once everything happened with my daughter though, I realized being a nurse was what I was meant to be. Therefore, I put myself through nursing school and am working on my bachelor’s degree today.
OCH: How long have you been with OCH? What drew you to OCH and what keeps you here?
KH: I’ve been with Option Care Health for 18 years. I originally started because of the nurse in charge of the business at the time. I respected her so much and decided I’d like to work for her so I joined the company and stayed because of the great people. Here in Norfolk, we’ve worked together for so long, we’re like a family.
EA: I initially came to Option Care Health because of the people – they just loved working here. I love having autonomy out in the field, not working 12-hour shifts but being able to help teach these patients when they have no idea what they’re doing or how they can do it at home, it’s just a rewarding aspect of nursing.
CG: I’ve been with Option Care Health for about four years, ever since I’d heard how rewarding infusion nursing was as a career. I had been doing dialysis but I was looking for something that would use both my technical skills and my bedside manner. This company has been so good to me; the people are extremely supportive and always make sure I have everything I need to do my job safely. I don’t feel like I’m working, I love it that much.
MB: I’ve been with OCH for about five years and I think I stay because of my manager and the people I work with. I also love my patients, I get to know them on a deeper, personal level and I’m able to help them because of the amount of time I’m able to spend with them.
OCH: In your opinion, what makes nursing at OCH special?
KH: Besides many of us being certified infusion nurses, we’re allowed to take the time we need with the patients to make sure they are comfortable. We’re able to do the teaching that allows them to be comfortable in their home or an Option Care Health Infusion Suite (AIS) with whatever therapy they are receiving.
EA: Everyone has the same goal. We work together as a team and we just want the same things no matter what area of the business you’re in. It’s all about the patient and making sure they’re taken care of – someone always has your back, people are open to ideas and you’re not alone out there.
CG: The term above and beyond exemplifies the nurses here. Every nurse will always go above and beyond to serve the needs of the patient and help the organization move forward. There’s nothing we wouldn’t do for our patients. I have an example, last week a nurse, Kim, came to New York City from Buffalo during height of COVID with bells and whistles on to help us for the week. That’s the kind of thing that makes OCH different.
MB: This is a unique environment that we all work independently, we’re not working side by side with our coworkers. However, I’ve never met any of our nurses that wouldn’t be willing to go the extra mile to help to provide the extraordinary care our patients deserve. That is truly unique to OCH and it’s very special to find people who are truly willing to help no matter what.
OCH: How do you plan to celebrate yourself during national nurses week?
KH: I haven’t really given it much thought. For me, what I do for peace and quiet is to go fishing.
EA: I don’t usually do anything because it’s my job, it’s all I’ve known. I just carry on and make sure the patients are taken care of, that’s my celebration. I don’t need recognition for something I enjoy doing, I truly get that when I’m caring for patients every day.
CG: I’ll probably do a Zoom with my family without interruptions. It may not sound like a lot but I just lost my grandmother over the weekend and taking time with my family that’s filled with joy amid all the negativity, it just fuels me. Even the fact that we’re social distancing and visiting in that way, it makes a big difference for me.
MB: Honestly, I don’t need any accolades or celebration, I truly enjoy what I do and it feels like it’s what I was meant to do. Being able to provide care for my patients is the only celebration I need.
OCH: What does it mean to you, to be providing extraordinary care during an unprecedented time like the one we’re currently in?
KH: I think for us, we have moved many of our patients into our infusion centers. I’ve been able to communicate with our patients and explain why coming to an AIS is lowering risk because of our cleaning procedures between patients. We are also able to lower the risk of exposure by not going into multiple houses to provide care. It’s the first time we’ve ever had to do this but it has been successful It’s working so far and we’re maintaining the health of our patients with their care at the forefront of what we do.
EA: I’m still able to get into the hospitals to teach but the biggest thing is not portraying fear to anyone. To me, the challenge is bridging the gap for the family and the patient. I had a patient the other day who was in the hospital for 11 days, alone. I had to help the family and the patient feel connected with their care, navigate the discharge process, manage the patient’s care after they returned home and help them believe that they successfully provide that care in their home.
CG: I build my happiness around my intentions. My intention is that every patient we care for comes away with an experience that was the same or better before COVID-19. Of course we are implementing safety measures that are different than before but I hope the quality of their care is being maintained or even better than before. I want Option Care Health to be known as a company that cares right now and throughout everything that happens after today.
OCH: What advice you have for people wanting to celebrate everything front line workers are doing during this pandemic?
KH: I enjoy the simple thank you’s. I am glad I’m a nurse, the most trusted profession; I just think the simple thank you’s go a really long way.
EA: What means the most to me is just saying thank you, you’ve made a difference and thank you. That’s all I need.
CG: This is a funny thing because when I got into nursing, I realized that my “applause” comes from within. When a patient is discharged, that is all I need to hear – Thank you for all you’ve done.
MB: I suppose, just a simple thank you. Honestly, that’s more than enough; I do what I do because I love what I do.
Globally, the nursing profession is celebrating a milestone in 2020, as the World Health Organization declares it the International Year of the Nurse and Midwife in honor of the 200th anniversary of the birth of Florence Nightingale.
Thank you for all you do for patients across the country today and every day. Happy Nurses Week.