Patient

Quince Therapeutics Selects Option Care Health as Specialty Infusion Therapy Provider for Administration of Lead Asset eDSP
August 7, 2025 (PDF Version)
Provides access to broad-reaching nationwide network of specialty pharmacy and ambulatory infusion suites across the U.S.
SOUTH SAN FRANCISCO, Calif. & BANNOCKBURN, Ill.–(BUSINESS WIRE)–Aug. 7, 2025– Quince Therapeutics, Inc. (Nasdaq: QNCX), a
late-stage biotechnology company dedicated to unlocking the power of a patient’s own biology for the treatment of rare diseases, today announced
that it has formed a strategic relationship with Option Care Health, Inc. (Nasdaq: OPCH), the nation’s largest independent provider of home and
ambulatory infusion services, to support the commercial development and efficient launch of Quince’s lead asset, encapsulated dexamethasone
sodium phosphate (eDSP) in the U.S., assuming positive study results and subsequent regulatory approval.
The strategic relationship will leverage Option Care Health’s robust network of specialty pharmacies and ambulatory infusion suites to provide for the
administration of eDSP in an effective and efficient way while delivering this innovative treatment to patients. With a national footprint of more than 90
full-service pharmacies and 180-plus ambulatory infusion suites located across the U.S., Option Care Health is well positioned to dramatically
enhance Quince’s ability to provide patients with Ataxia-Telangiectasia (A-T) access to eDSP treatment, including greater geographic flexibility to
match patient locations and eDSP administration needs, an improved and standardized patient journey with higher control and consistency across
eDSP administration sites, the benefit of contracting with a single provider versus multiple individual academic centers of excellence, and scalability to
treat patients in additional targeted indications such as Duchenne muscular dystrophy (DMD). Additionally, the engagement will be supported by
Option Care Health’s comprehensive suite of enhanced service capabilities, including third-party logistics (3PL) and inventory distribution
management, program management, customized patient registration and hub support, clinician-delivered services, physician reporting, and data
collection and reporting.
Charles Ryan, J.D., Ph.D., Quince’s President who manages several departments including Commercial, said, “We are very pleased to enter into a
strategic partnership with Option Care Health that is designed to greatly improve the patient journey while also establishing an effective and efficient
commercialization pathway for our highly innovative lead asset, eDSP. Option Care Health is a strong partner with a deep understanding of the
complexities of rare disease treatments. We look forward to working together to leverage all the benefits of its nationwide integrated care platform of
specialty pharmacy, infusion suites, and nursing services for the benefit of patients with A-T.”
Eric Daugherty, Senior Vice President, Biopharma Relations, of Option Care Health, said, “As a leading provider in the treatment of rare and orphan
diseases, our organization is honored to have been selected by Quince as its specialty infusion therapy partner. Together, we are committed to making
their novel eDSP asset accessible for patients with A-T across the U.S. as Quince readies for commercial launch and ultimately looks to engage
providers and payers in a seamless way.”
About Quince Therapeutics
Quince Therapeutics, Inc. (Nasdaq: QNCX) is a late-stage biotechnology company dedicated to unlocking the power of a patient’s own biology for the
treatment of rare diseases. For more information on the company and its latest news, visit www.quincetx.com and follow Quince on social media
platforms LinkedIn, Facebook, X, and YouTube.
Forward-looking Statements
Statements in this news release contain “forward-looking statements” within the meaning of the Private Securities Litigation Reform Act of 1995 as
contained in Section 27A of the Securities Act of 1933, as amended, and Section 21E of the Securities Exchange Act of 1934, as amended, which are
subject to the “safe harbor” created by those sections. All statements, other than statements of historical facts, may be forward-looking statements.
Forward-looking statements contained in this news release may be identified by the use of words such as “believe,” “may,” “should,” “expect,”
“anticipate,” “plan,” “believe,” “estimated,” “potential,” “intend,” “will,” “can,” “seek,” or other similar words. Examples of forward-looking statements
include, among others, statements relating to the benefits of the strategic partnership with Option Care, including improved patient access and other
commercial development activities; current and future clinical development and regulatory approval of eDSP, including for the potential treatment of
Ataxia-Telangiectasia (A-T), Duchenne muscular dystrophy (DMD), and other potential indications; the strategic development path for eDSP; planned
regulatory agency submissions and clinical trials and timeline, prospects, and milestone expectations; and the potential benefits of eDSP and the
company’s market opportunity. Forward-looking statements are based on Quince’s current expectations and are subject to inherent uncertainties,
risks, and assumptions that are difficult to predict and could cause actual results to differ materially from what the company expects. Further, certain
forward-looking statements are based on assumptions as to future events that may not prove to be accurate. Factors that could cause actual results to
differ include, but are not limited to, the risks and uncertainties described in the section titled “Risk Factors” in the company’s Quarterly Report on Form
10-Q filed with the Securities and Exchange Commission (SEC) on May 13, 2025, and other reports as filed with the SEC. Forward-looking statements
contained in this news release are made as of this date, and Quince undertakes no duty to update such information except as required under
applicable law.
View source version on businesswire.com: https://www.businesswire.com/news/home/20250807215445/en/
Media & Investor Contact:
Stacy Roughan
Quince Therapeutics, Inc.
Vice President, Corporate Communications & Investor Relations
ir@quincetx.com
Source: Quince Therapeutics, Inc.

Patient
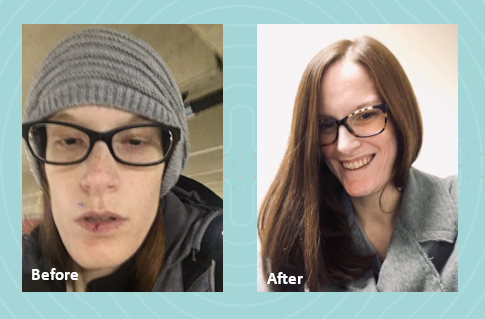
In 2022, I graduated from nursing school with dreams of starting my career as a nurse. However, life had other plans. I was diagnosed with gastroparesis, a condition that made it impossible for me to work and pursue my passion. As my condition worsened, I had to put my career on hold to focus on my health.
 Initially, my local clinicians recommended jejunal feedings, which I tolerated well at first. However, after my J-tube surgery, my condition began to deteriorate, and eventually I became severely malnourished. I was surviving on a mere 500 calories a day, leaving me too weak to perform even the simplest tasks. My mom had to help me with everything, including bathing. Living in a two-story home became a daily struggle, as I had to crawl up the stairs, feeling my body slowly giving up.
Initially, my local clinicians recommended jejunal feedings, which I tolerated well at first. However, after my J-tube surgery, my condition began to deteriorate, and eventually I became severely malnourished. I was surviving on a mere 500 calories a day, leaving me too weak to perform even the simplest tasks. My mom had to help me with everything, including bathing. Living in a two-story home became a daily struggle, as I had to crawl up the stairs, feeling my body slowly giving up.
My local registered dietitian recommended Parenteral Nutrition (PN) and sent the order. We were then referred to Option Care Health (OPCH). I was scared to start PN, but my OPCH dietitian reassured me, saying, “Just because you’re on PN doesn’t mean your life is over. The goal is to give you back more of your life than before.” Her words stuck with me, offering hope during a difficult time.
Due to my blood sugar issues, I’m on 23-hour PN feeds and carry a backpack that has become a part of me. Despite these challenges, my OPCH team has been incredible. My registered dietitian and pharmacist have truly been lifesavers. I continue to speak with my OPCH registered dietitian weekly because she genuinely cares about my well-being and supports me through every step of my journey.
Thanks to the unwavering support of my Option Care Health team and my local registered dietitian, I am back to work and feeling so much better. I wholeheartedly recommend Option Care Health to anyone in need. They have played a crucial role in my recovery, and I am forever grateful for their dedication and care.

Patient
Gastroparesis refers to a delay in emptying stomach contents. Symptoms often include feeling full after eating a meal, or even a small amount of food, as well as nausea, vomiting, bloating or abdominal pain. The causes of gastroparesis may include diabetes mellitus, complications after surgery, kidney disease, certain medications, thyroid disorders, cancer, among others.
The following tips are intended to reduce symptoms and help maintain adequate nutrition.
|
Mealtime
|
||
|
Foods
|
|
|
Fluids
- Stay hydrated. Most adults need 6-10 cups of water per day. Sip slowly throughout the day.
- Drink fluids with meals, however; be sure not to fill up on liquids
- Avoid carbonated beverages as they can cause bloating
Other
- Avoid alcohol as it can affect stomach emptying
- Foods that are acidic, spicy, or contain caffeine or mint may increase acid reflux
- Keep blood sugars under control if you have diabetes
- Keep a food diary to track your intake and find foods that are best tolerated
- Exercise may increase stomach emptying and reduce symptoms. Walking after meals is suggested.
See below for help in choosing more optimal foods from each food group:
 |
|
Gastroparesis Sample Menus |
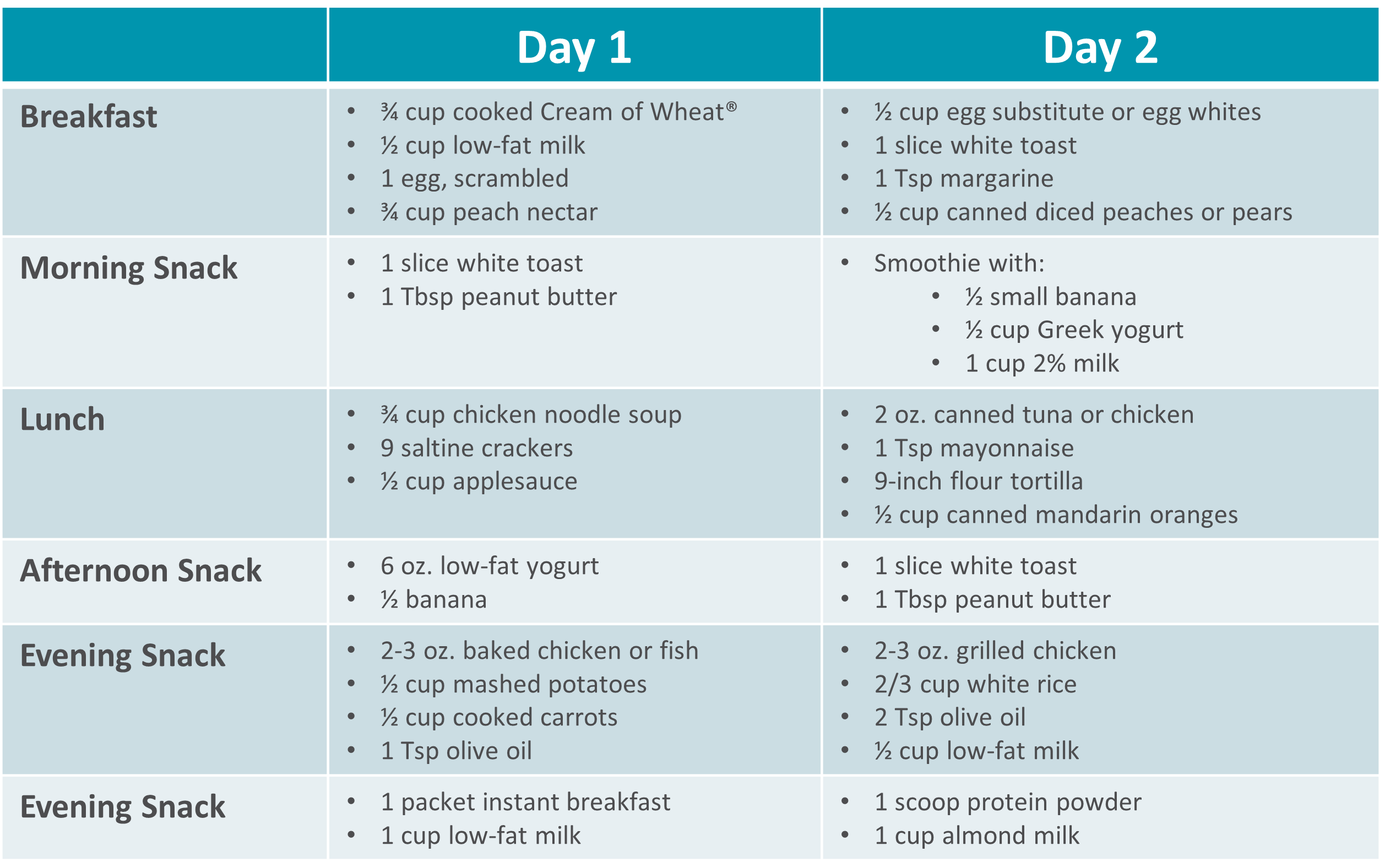 |
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health.
*This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information.

Patient
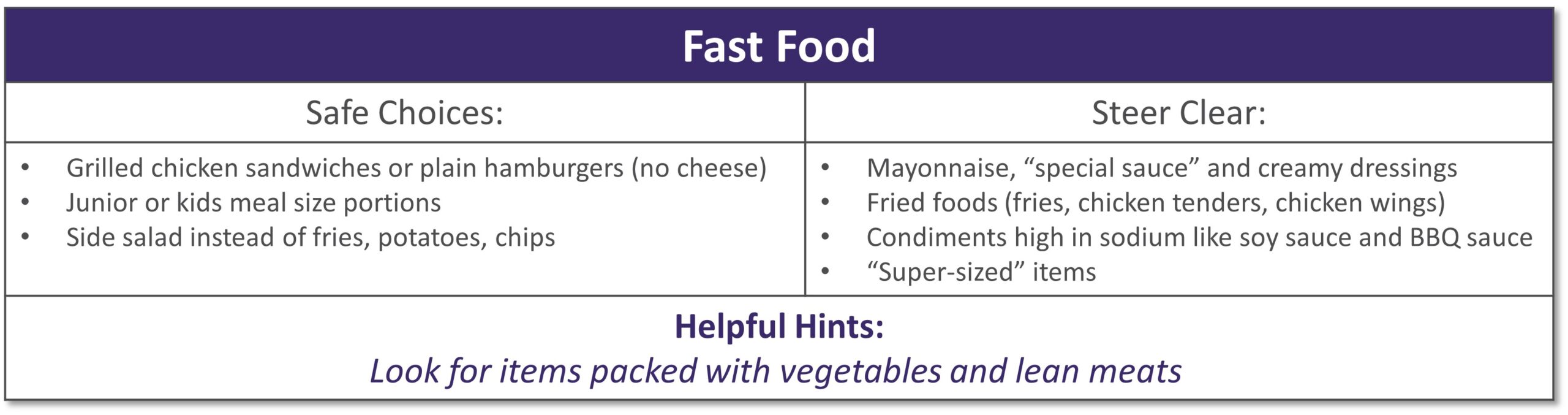
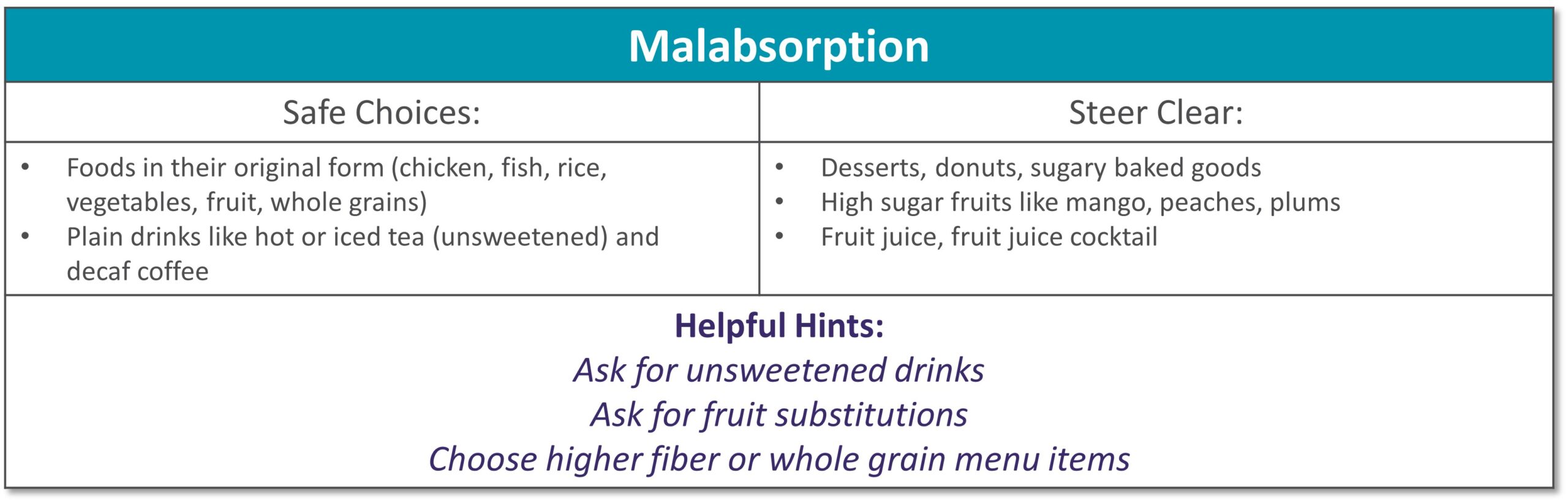
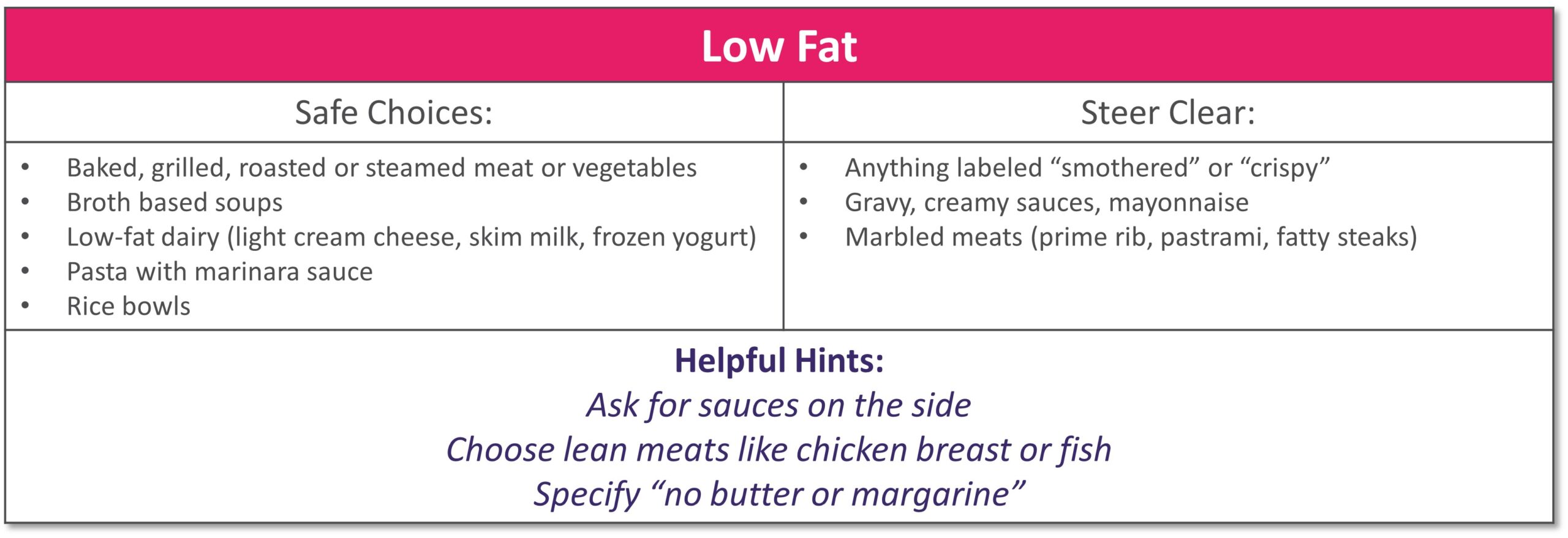
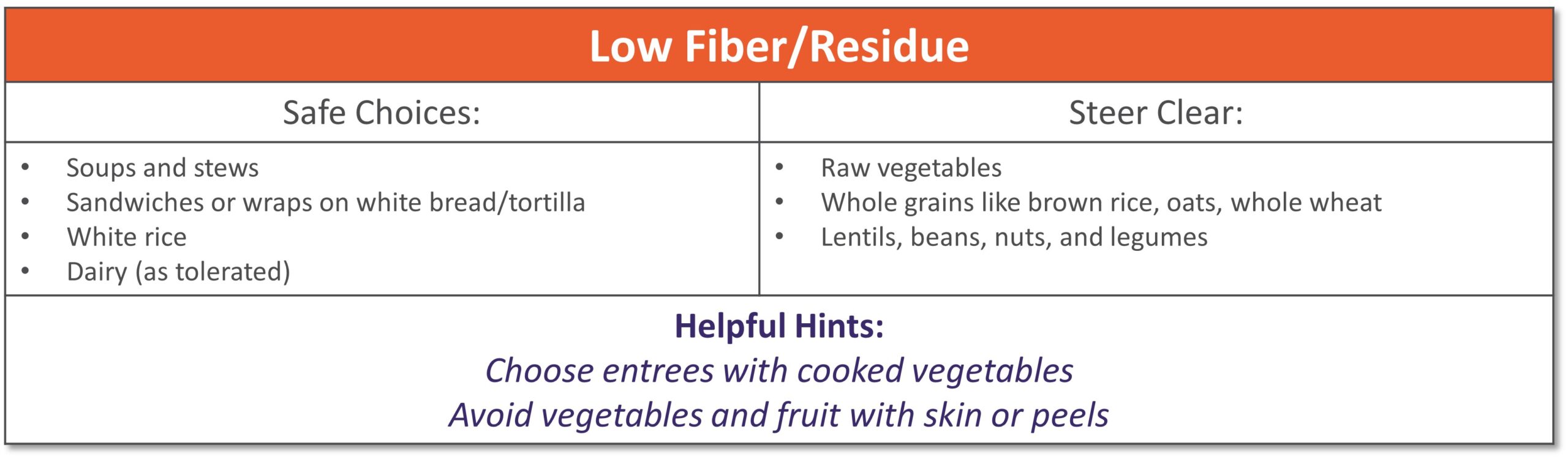
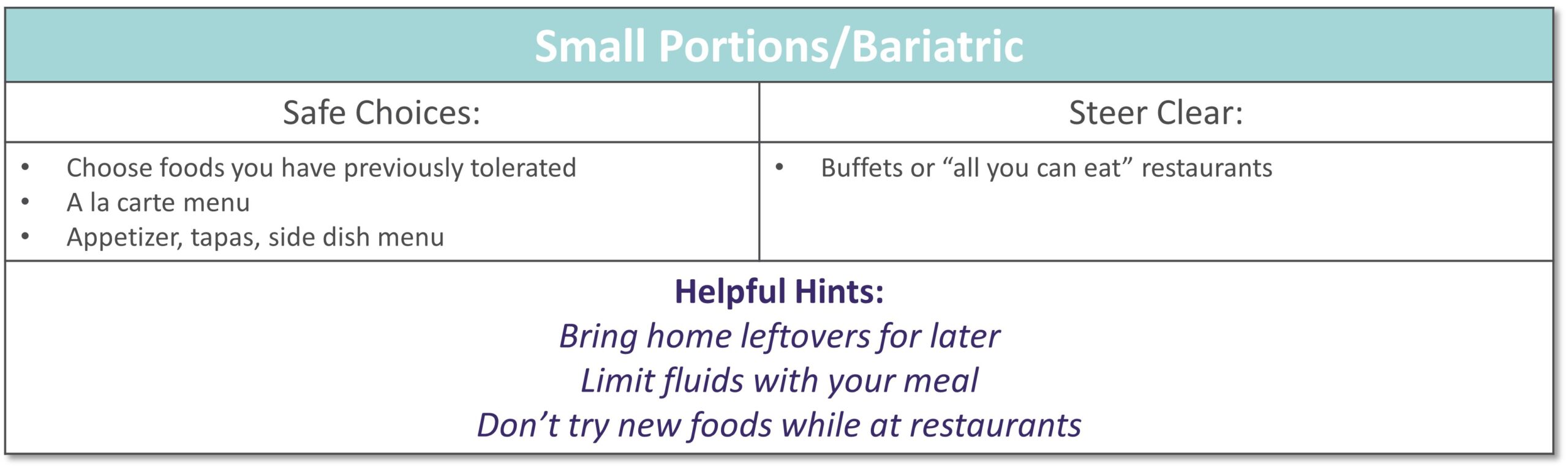
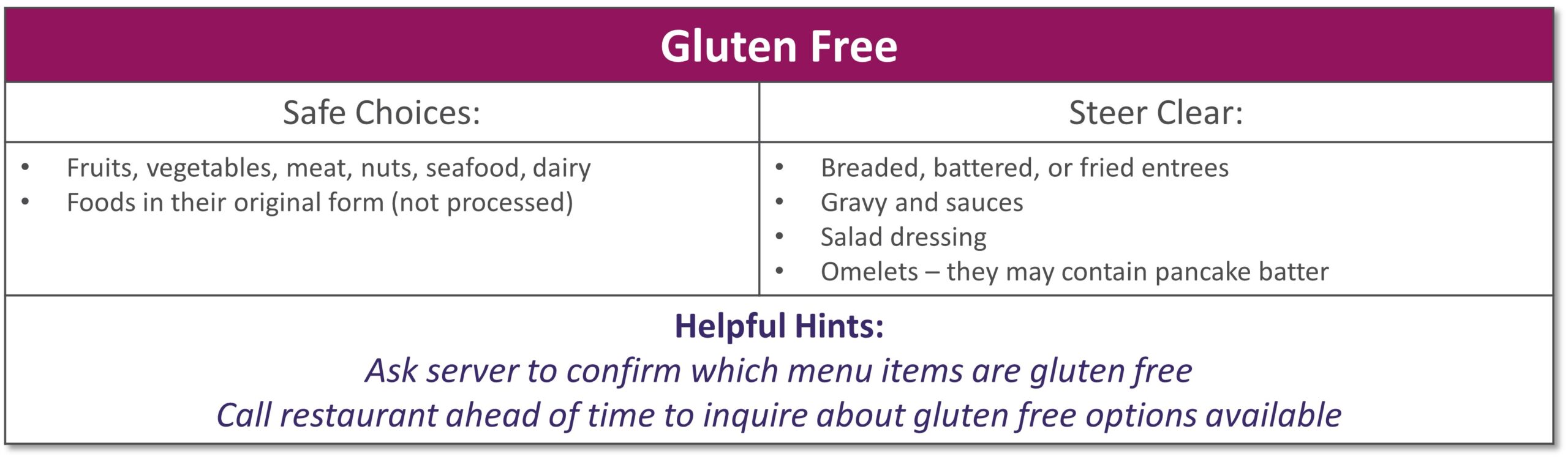
Dining out at restaurants is a nice treat but also challenging when trying to stick with your therapeutic diet, especially with gastrointestinal diseases. Most restaurants have menus and nutritional information available online. Restaurants are not required to have nutrition information available if they have less than 20 locations. Follow these tips to navigate eating out if you have specialized nutrition needs.
GENERAL TIPS:
- Research the menu online
- Pick a cuisine you tolerate
- Ask server for nutritional information or ingredients if not listed on the menu
- Do NOT be afraid to ask to customize the meal or ask for specific changes
- Communicate with wait staff if you have a food allergy or intolerance
- HAVE A PLAN AND STICK WITH IT!
|
|
|
|
|
|
|
|
|
|
|
|
|
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health. *This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information. |

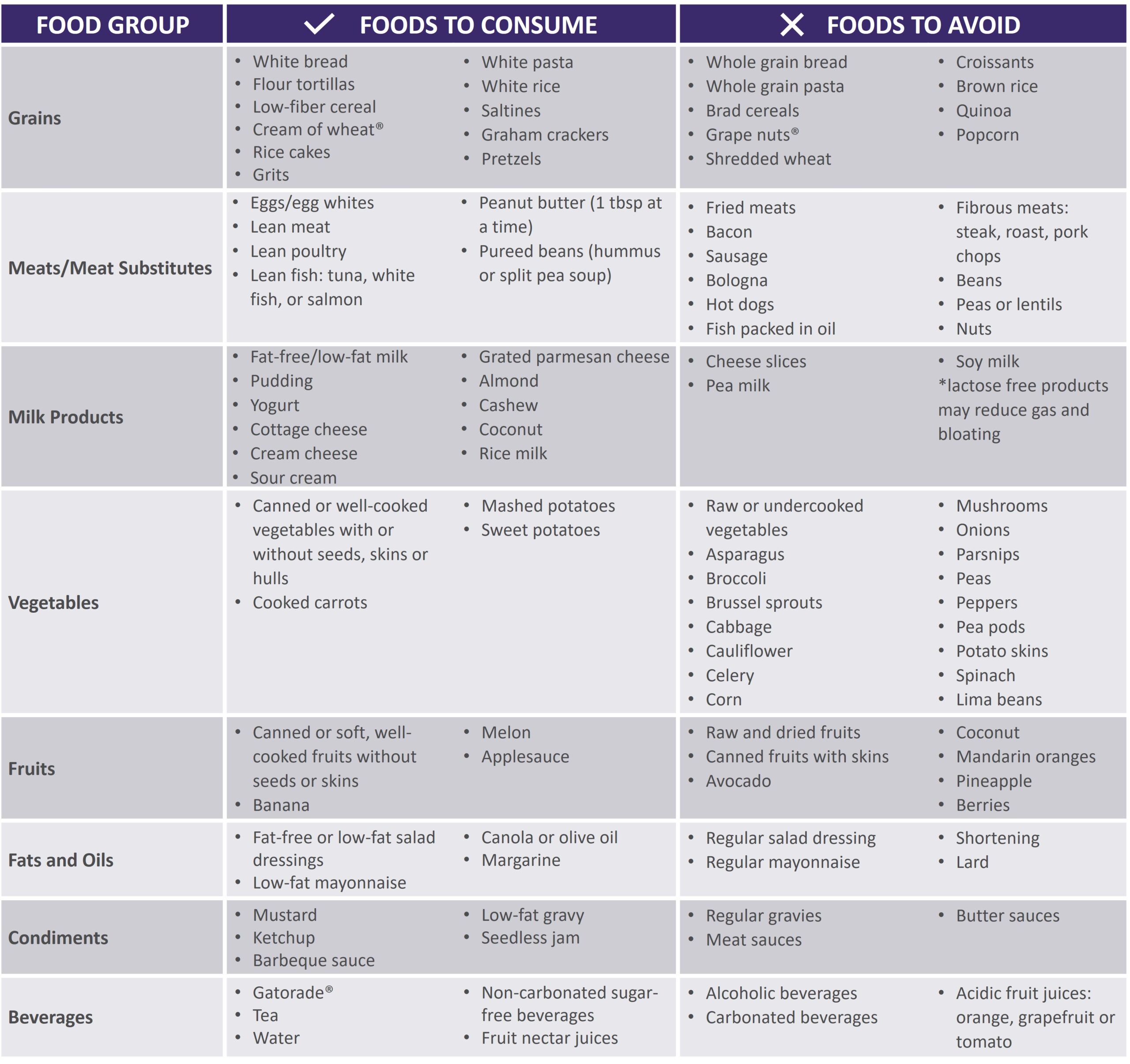
Patient
Short bowel syndrome (SBS), or intestinal failure, is a condition in which your body is unable to absorb enough nutrients from foods and fluids you consume. This can occur after a surgical resection or damage to your intestines. Symptoms and absorption vary by individual based on the amount and health of the remaining intestine. Symptoms of SBS can include diarrhea, dehydration, electrolyte abnormalities, and weight loss.
The following tips are intended to maximize absorption, improve your nutritional status and reduce dependence on parenteral nutrition.
- Mealtime
- Eat small, frequent meals (6-8 per day)
- Foods
- Eat protein at all meals: eggs, creamy peanut butter, chicken, fish, beef, tofu
- Choose complex carbohydrates such as bread, pasta, rice, and potatoes
- Limit raw vegetables to small amounts
- Avoid fruits with skin or edible seeds
- Limit raw fruits to very small portion twice a day
- Increase your soluble fiber to thicken output with foods such as bananas, applesauce, rice, oatmeal or use of soluble fiber supplements
- Avoid high fat foods such as fried foods if your colon is intact
- Use caution with dairy products – lactose intolerance is common with SBS
- Avoid concentrated sweets such as candy, desserts, and juice
- Avoid foods artificially sweetened with sorbitol or mannitol (Splenda® is okay)
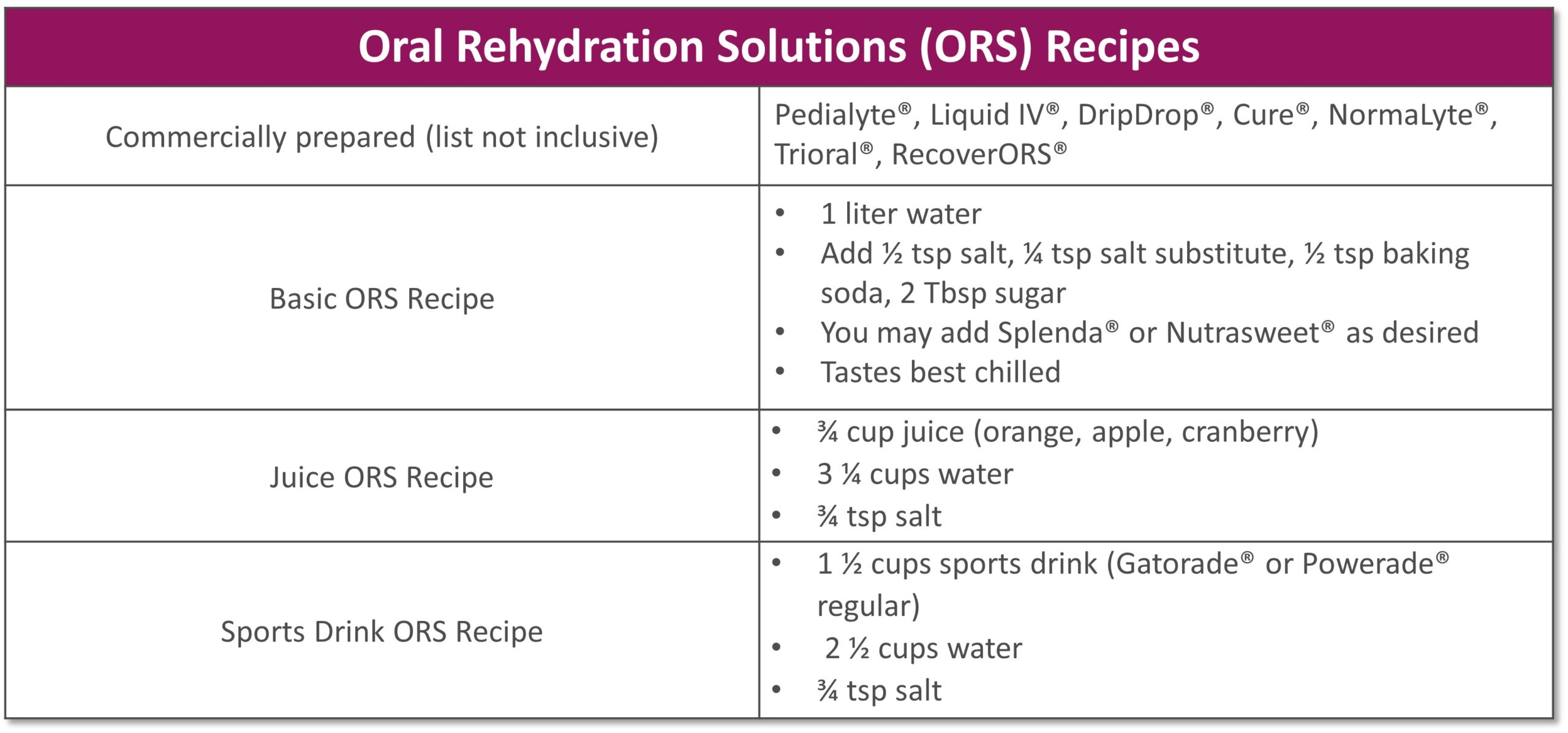
- Fluids
- Drink isotonic fluids (with electrolytes), ideally oral rehydration solutions (see recipes below)
- Do not drink fluids with meals as it increases how quickly food passes through
- Limit to 4 oz. fluid during your meal to allow your food to be best absorbed
- Drink ½ hour before or 2 hours after eating
- If you do not have your colon, your fluid losses will be higher
- Other
- If prescribed by your doctor, take antidiarrheal medication ½ hour before meals
- Salty foods such as pretzels or soups are usually well tolerated and help absorb fluid
- Avoid caffeine and alcohol
See below for help in choosing more optimal foods from each food group:
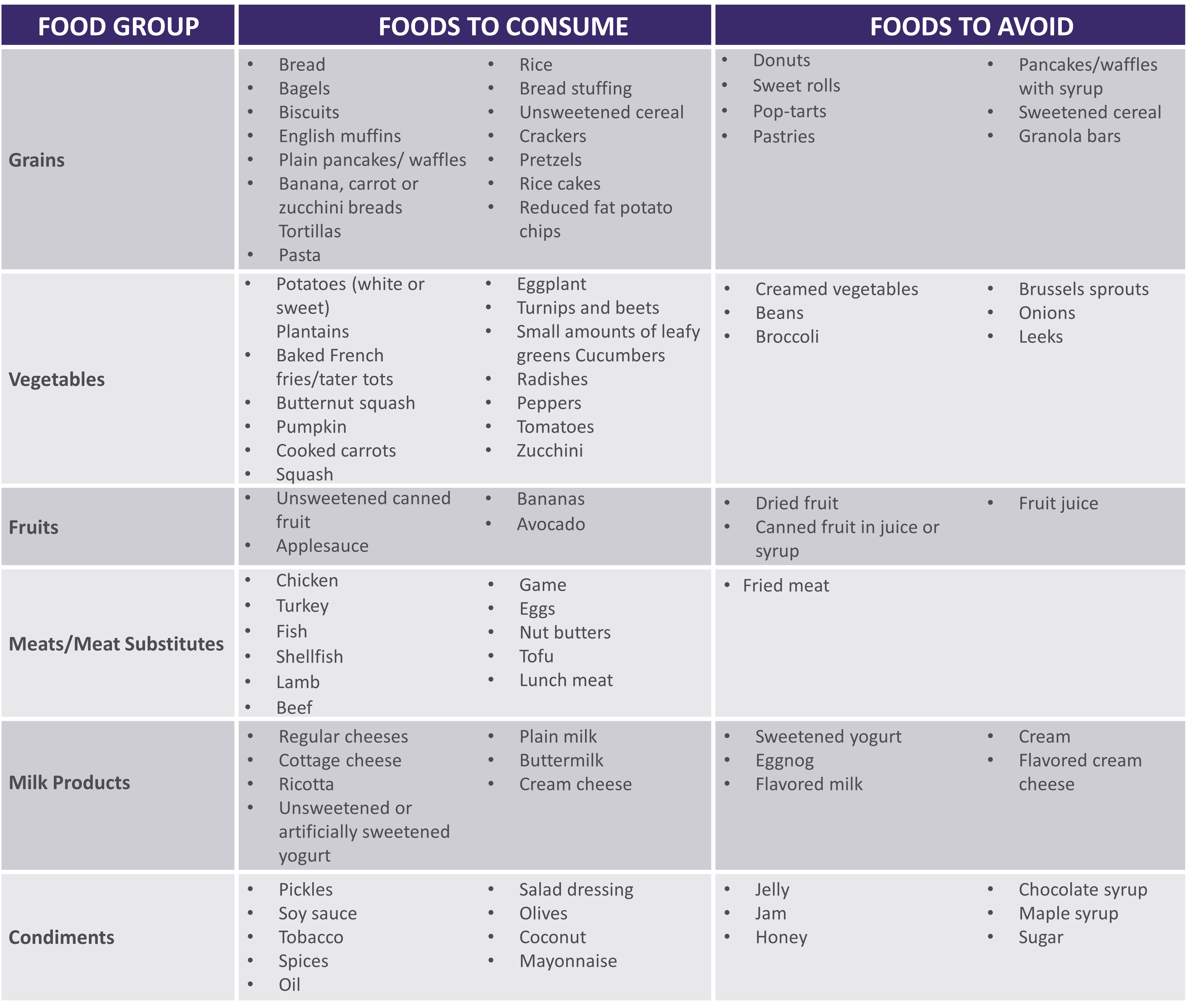 |
|
|
|
**For homemade ORS, discard after 24 hours if not consumed **Visit for more recipes: https://optioncarehealth.com/patients/resources/sbs-friendly-recipes |
SBS Sample Menu |
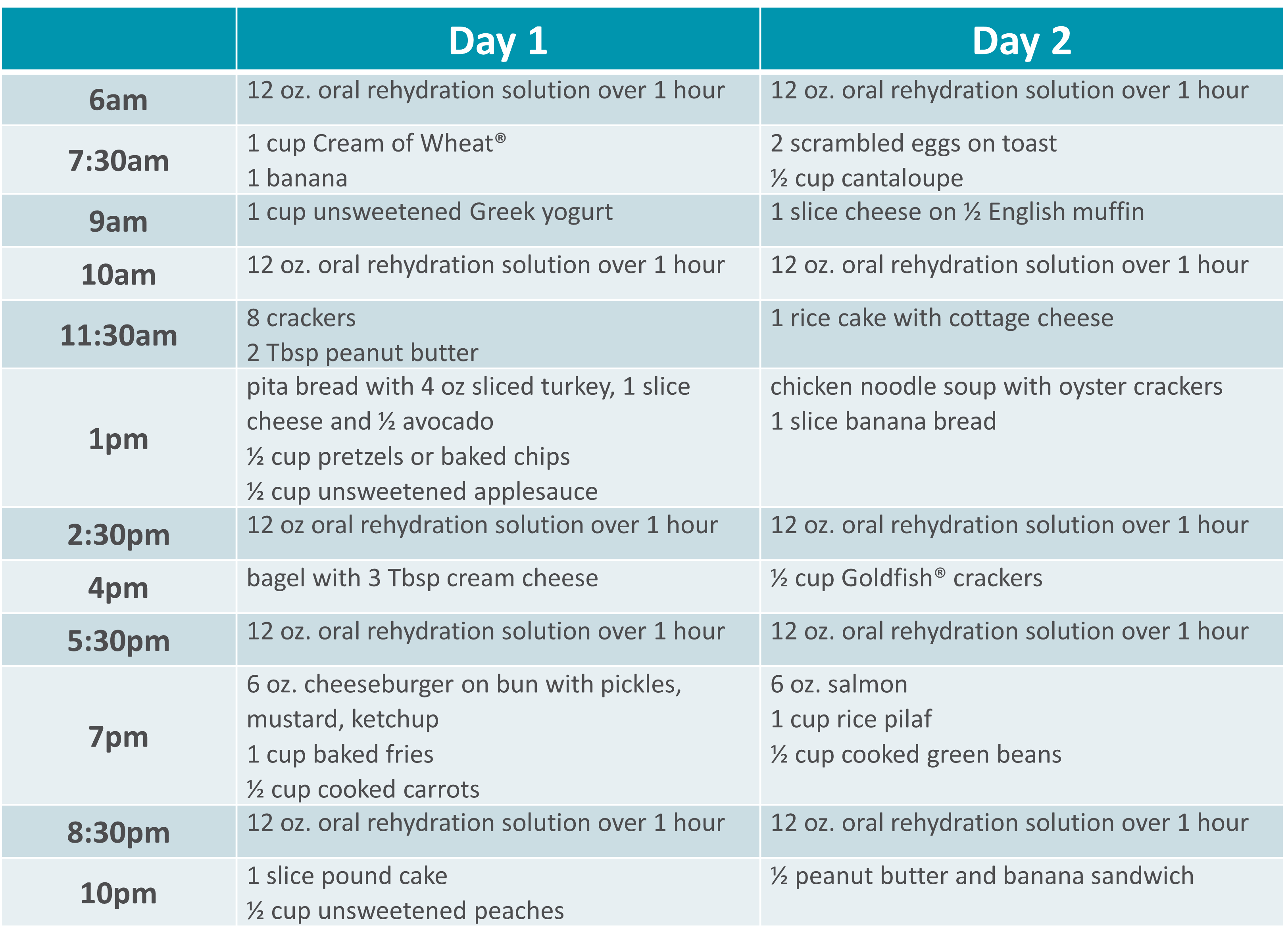 |
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health.
*This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information.

Patient
Gillian was just 11 years old when she began treatment for multiple complex chronic illnesses. As a teenager, she was diagnosed with gastrointestinal (GI) motility disorder and gastroparesis, which led to long-term, severe malnutrition.
“It was really hard missing out on so many activities growing up. I was prescribed various medications and tube feedings, but nothing helped long term. By early adulthood my symptoms worsened so I had to withdraw from college and take an extended medical leave from my job,” she said.
From 2015 to 2018, Gillian’s health progressively declined. “I was on tube feeds and other intravenous (IV) medications at the time. I began losing weight again, my neurological function was declining and I couldn’t speak or walk.” As Gillian’s health continued to decline, she found the strength to advocate for herself and build upon her excellent team of healthcare providers.
Gillian was put on total parenteral nutrition (TPN) in 2018, managed by Option Care Health. “This was my turning point. Today my labs are perfect and my cognitive function is back to normal. My weight has stabilized and I’m back to living life. I owe so much of my progress to my Option Care Health team.” Gillian continued, “My registered dietitian (RD) is amazing. During the initial COVID outbreak, I was struggling with my health and I couldn’t reach my doctors, but my Option Care Health RD was there every time I reached out. I got the help I needed and I owe it all to her.”
She claims that her Option Care Health team including her pharmacist and pharmacy technician go above and beyond expectation. “Other companies and even providers don’t always focus on how the patient needs to be living their best quality of life during treatment. My team at Option Care Health set up my deliveries in the evening to accommodate my work schedule. They also deliver them upstairs to me because I’m unable to carry them. My pharmacist and tech were so helpful this summer. They were able to find a way for me to go on vacation by switching around my infusions and supplies. Thanks to their help, I was able to go on my first trip since 2015! They are really focused on me as a person, not just a patient.”
Her message to her Option Care Health team is one of gratitude, “I just want them all to know how appreciative I am. They have and continue to be a key part of my recovery and I couldn’t be more grateful.” Gillian is thriving and living her best quality of life. She’s working, volunteering and spending as much time as possible with family and friends.
Learn more about malnutrition and join us in spreading awareness this ASPEN Malnutrition Awareness Week*, September 19th-23rd: ASPENMAW22
*Malnutrition Awareness Week™ is a mark of the American Society for Parenteral and Enteral Nutrition (ASPEN). Used with permission from ASPEN.

Patient
As a leading healthcare provider, we recognize our role and our responsibility to protect the health and safety of our patients, customers, team members and community. Option Care Health is mandating all leaders be fully vaccinated by September 30, 2021 and all patient and customer-facing team members be fully vaccinated by October 15, 2021.
“Our mission is to transform healthcare while delivering hope to our patients and their families,” said John Rademacher, Chief Executive Officer. “We believe our single largest contribution to eradicating COVID-19 is through vaccination. By receiving the vaccine, we are becoming a part of the solution. Each one of us at Option Care Health plays a critical role in our purpose of providing extraordinary care that changes lives.”
Option Care Health complies with applicable federal, state and local laws and will evaluate exceptions to the vaccine requirement due to a medical condition or strongly held religious beliefs.

Patient
Four years ago, Sherry Hambly, 56, developed a painful rash, that constantly felt as if she had a terrible sunburn. Her skin burned every time she washed her hands or took a shower and her muscles were weak. After a long journey searching for answers, she was diagnosed with dermatomyositis, an autoimmune disorder. She’s now receiving intravenous immunoglobulin (IVIG) at the Option Care Health Infusion Suite in Troy, Mich., and is grateful to have her life back.
Prior to finding the right diagnosis and treatment, Sherry was so uncomfortable she had to take pain medicine daily and could barely perform her job as an accountant, due to weakness. She didn’t sleep well and was too exhausted to relish the things that brought her joy, including playing with her grandchildren, golfing, bowling and doing yoga.
“I love the employees at the Troy infusion suite because I never have to lift a finger – they take care of everything and made sure my care plan was personalized for me,” said Sherry, of Rochester Hills, Mich.
Early on, she was taking hydroxychloroquine, a high dose of steroids and an anti-rejection drug. Her original IVIG prescription involved four-hour IVIG infusions three days in a row once a month, but by the end of the month the benefits wore off and she didn’t have the energy to go to the office. The Option Care Health team worked with Sherry, her doctor and pharmacist to devise a care plan that worked best for her and she now receives the infusions two days a week every other week.
“It’s made all the difference in the world,” she said. “I no longer take any pain pills and am completely off all the steroids I relied on to keep me moving, because my IVIG treatment is helping so dramatically.”
She lives with her husband, son and two grandchildren. Now that she has her energy back, she’s able to assist her 11-year-old grandson with his home schooling and watch her 16-month old granddaughter. She’s back to golfing and doing yoga and can perform her job to her fullest potential.
“I really like the infusion suite – it’s nice being in your own little space during COVID-19 – the room has windows, comfortable chairs and a kitchen where I can warm up my coffee. It’s quiet and I can even work while I’m there,” she said. “The staff is always going above and beyond to make sure we’re safe and comfortable.”

Patient
Frequently ill with pneumonia, bronchitis and other serious infections, Cambria Hooven, 35, limited her contact with people and didn’t leave her house much. After finally learning the reason for her near-constant sickness was a weakened immune system due to common variable immune deficiency (CVID), she began receiving intravenous immunoglobulin (IVIG) at home through Option Care Health. She felt free to get out more and socialize, but then the COVID-19 pandemic hit.
Because Cambria was afraid to risk having visitors come to her home, her Option Care Health nurse, Kola devised a plan. He suggested she receive treatments at the Option Care Health Langhorne Infusion Suite where he works, which is a 35-minute drive from her home in Philadelphia.
“I was nervous about it as I hesitate to go anywhere during this pandemic, so he sent me a video of the suite before my first appointment, walking through everything and showing me exactly what doors to enter,” said Cambria, who gets teary eyed at the memory. “Kola has been my nurse for two years and he’s like family to me. I don’t know what I would do without him in my life!”
She now receives her four-hour monthly treatments in a clean and sanitized room, which has its own comfortable lounge chair and large windows. Because she otherwise stays home during the pandemic, she really enjoys going for her monthly infusions. “It’s a little retreat center,” says Cambria.
Cambria is relieved to finally have a diagnosis and receive treatment. For years, she saw one doctor after the next to try to figure out why she was always sick. Eight years ago, she had her appendix removed, got a serious blood infection and spent 33 days in the hospital, unsure if she would survive. Determined to get to the bottom of her problem, she took a leave from her job as a social worker in child welfare to have one test after the other.
She finally saw an immune specialist who diagnosed her condition and prescribed IVIG. As a result, she hasn’t been hospitalized since. Initially, she began self-infusing at home, but wasn’t comfortable with it. Option Care Health recommended a nurse come to her home to provide the infusions and that’s how she met Kola.
Now that she’s receiving treatment, Cambria feels healthier and is able to do her work as a social worker remotely, often from the Langhorne infusion suite.
“I know how to stay safe and the treatment I get at Option Care Health helps so I don’t have to live in fear and isolation. I can get outside safely to hike and backpack,” she said. “It’s great going to the Langhorne suite, which is safe and clean and I have so much respect for the nurses and their families. They’re so considerate.”

Patient
Abbi Tucker’s simple wish is to be a normal teenager and enjoy playing music, but when she was 13, severe migraine headaches and terrible stomach aches, that resulted in a 50-pound weight loss, derailed her hopes for a while. After numerous tests and consultations with doctors she was diagnosed with Crohn’s disease, an inflammatory bowel disease. Her life is back on track now that she receives infusions of therapy treating chronic inflammatory disorders at Option Care Health’s Troy Infusion Suite.
“Once I started getting treatment, my life changed,” says Abbi, now 16, of Marysville, Mich. “I gained the weight back and could finally focus on school and having fun again.”
When Abbi started experiencing severe health issues, she and her family were frightened and she was miserable. Her symptoms caused her to miss at least one day of school a week and she found it difficult to keep up with her studies. She couldn’t hang out with her friends, play or teach piano, and even lost her appetite.
Now with a treatment plan in place, she’s back to her activities, including band practice as a junior drum major, spending time with friends and playing music at her church. Eating is also gratifying, although she stays away from greasy and spicy foods as well as popcorn.
Abbi originally received her one-hour therapy every seven weeks at the hospital. When insurance issues arose necessitating a switch to an infusion company, she and her family selected Option Care Health and couldn’t be happier with their choice.
“I LOVE the nurses there,” she said. “I have a hard time getting my blood going for blood draws, which made them painful. One of my Option Care Health infusion nurses made me a heating pad and I use it every time I get my blood drawn. It’s amazing.”
Antonette, the receptionist at the facility, calls to remind her family about upcoming appointments and the staff knows to look for her dad’s red truck when she gets dropped off. He’s a fireman and paramedic with a medical background, which puts her family at ease.
She likes getting her care at the infusion suite instead of at home because she occasionally has had adverse reactions. She takes Benadryl and a steroid before every treatment, which helps, but she’s comforted to know that Option Care Health nurses are nearby if she starts having issues. She also appreciates the privacy of the suites.
“The staff always makes me feel right at home and that my health is their number one priority,” said Abbi. “Infusion therapy really has been lifechanging and now I can do what a typical 16-year-old would do every day.”